By Boris GOJANOVIC (@DrSportSante), Aurélie DELACROIX-TARENNE, Guillaume LACHAUX-COUTTET, François FOURCHET (@FFrunsanteperf).
The coronavirus pandemic is growing fast and forcing us to rethink how we approach medical care. Face-to-face consultations are no longer recommended for non-urgent complaints (situation in Switzerland on March 20th), for all allied health professionals, in particular physiotherapists. “Stay-at-home” is the mantra, which means that clinicians working outside of emergency services must act as exemplary leaders to prevent the spread of COVID-191. This situation is new to our digital world, outside of localized war zones, and the sheer magnitude of the pandemic is frightening, although many seem to minimize the risk.
DUTIES AND OPPORTUNITIES
With every challenge come duties and opportunities. Our duty as medical professionals in sports and exercise medicine (SEM) is to–like every healthcare professional–make public health a priority. We also have a duty of care to our patients. This is where the challenge comes. How do we continue looking after our athletes? We are used to going the extra mile for them, but now we work in a different reality, one where the human coronavirus treats all humans equally.
And, what about the general population? Most of the complaints seen at a clinic, whether musculoskeletal or exercise limitations for medical reasons, end up not being addressed or not being treated, as long as it does not pose an imminent threat. Many could actually benefit from the current crisis. People will have to stay off some irritating activities, and have time by default to do their at-home exercises — you know, the ones they never really do. We can help them by implementing existing telehealth strategies2,3.
TELEHEALTH IN SPORTS AND EXERCISE MEDICINE
This is the opportunity to deploy our elite sports modus operandi. Sports science and medicine is our field laboratory, which we use to improve care for the rest of the population. Training and rehabilitation principles are universal, whatever the level of fitness. Our expertise in SEM applies across the board. SEM physicians must regularly manage the health of athletes from a distance, relying on history taking, images and videos: when your athlete is training in Iten (Kenya), he/she has got you and his/her smartphone to help. Enter telemedicine in the current coronavirus lock-down.
THREE WAYS TO ADAPT TO TELEMEDICINE DURING THE COVID-19 PANDEMIC
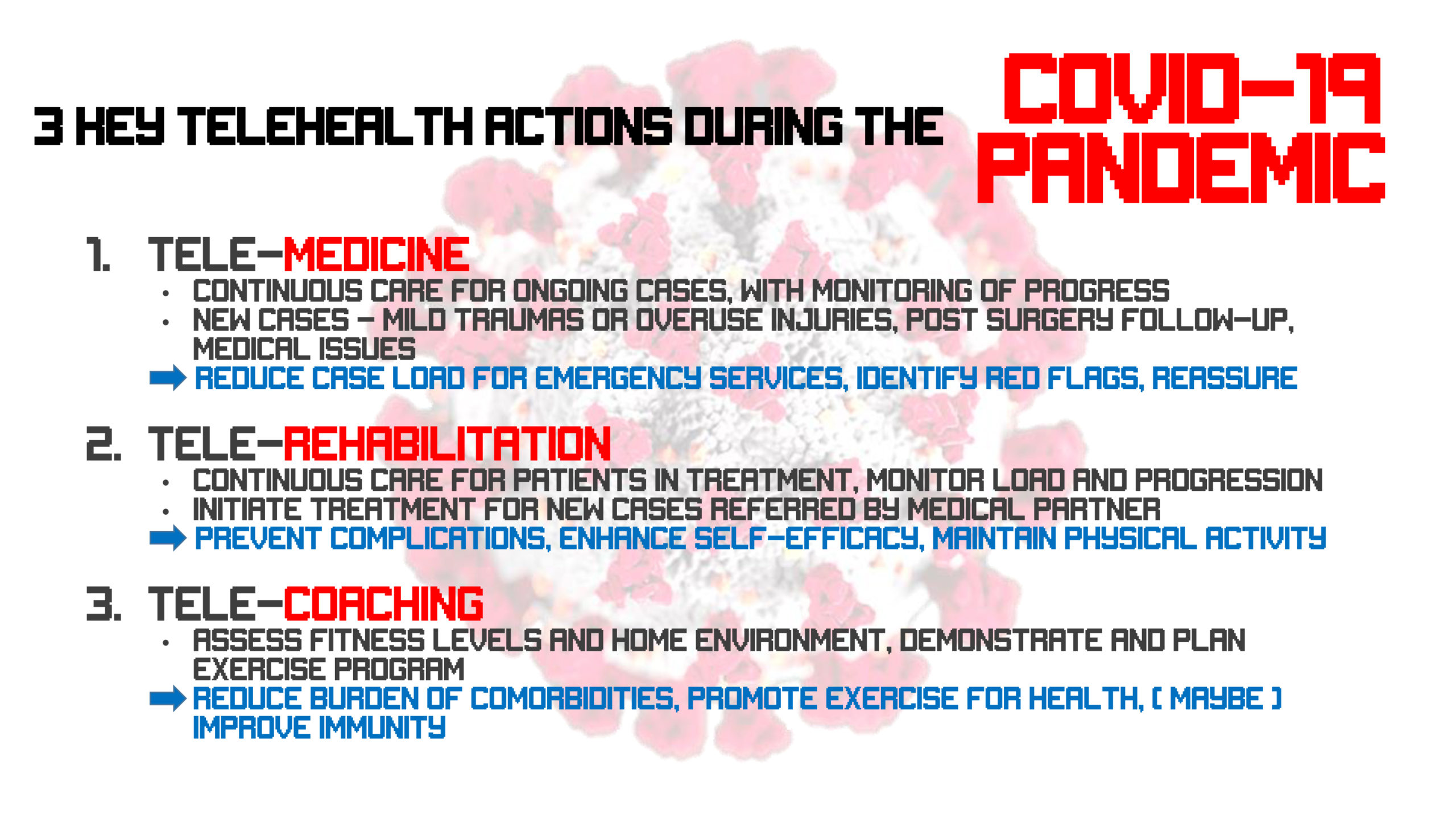
We implemented three things quickly as soon as the first “stay-at-home” messages came out: tele-consultation, tele-rehabilitation and tele-coaching (Figure 1).
Figure 1: The three telehealth actions during COVID-19
The medical doctor can establish a functional diagnosis for most musculoskeletal complaints, ruling out red flags, and conducting a screen-based physical examination. A working diagnosis will, by definition, not be structure-based, but function-based.
From there, our rehabilitation specialists (physiotherapists) organize interactive sessions through the screen, exercise prescription and supervision, and follow the patients for exercise progression and load monitoring — hands-off treatment4.
When the needs are not for a specific rehabilitation issue, we engage our strength and conditioning staff to assess current physical activity, at-home training options, and introduce coaching for general health maintenance or improvement. Patients receive a progressive and tailored training program. We encourage people to stay active in these times of lock-down, within the limits of their homes, hoping that some will kick-start a healthy exercise routine during COVID-19 times.
Regular physical activity reduces the incidence of viral infections by 50% through various immunity-enhancing mechanisms5. Studies have looked at upper respiratory tract infections caused by “common cold” viruses (4 coronavirus strains are part of them) There is no evidence that the immunity against SARS-CoV-2 is also improved, but it might be. We recommend to stay active regularly to offset the newly imposed sedentariness whilst avoiding strenuous activities (evidence exists that it temporarily reduces immunity). For SEM practitioners, stay tele-active to help your athletes, patients and the general population. Emergency services will be thankful, as you will contribute to reduce unnecessary visits and use of much needed resources.
***
Authors
Boris GOJANOVIC1,2, Aurélie DELACROIX-TARENNE1, Guillaume LACHAUX-COUTTET1,3, François FOURCHET1
1Hôpital de La Tour, Sports Medicine and Physiotherapy Department, Swiss Olympic Medical Center, Meyrin (GE), Switzerland
2Consultation SportAdo, Department for Woman, Mother and Child (DFME), Lausanne University and Hospital, Lausanne, Switzerland
3Master STAPS Entrainement et optimisation de la performance sportive, Université Grenoble Alpes, Saint-Martin-d’Heres, Rhône-Alpes, France
The author team represents the medical, physiotherapy and strength and conditioning staff of La Tour Hospital (Geneva, Switzerland), a Swiss Olympic medical center dedicated to health in general, movement and sports performance in particular. Email: boris.gojanovic@latour.ch
Competing interests
None
References
- Hollander JE, Brendan GC. Virtually Perfect? Telemedicine for Covid-19. New England J Med. Mar 11. doi: 10.1056/NEJMp2003539.
- Tenforde AS et al. Telehealth in Physical Medicine and Rehabilitation: A Narrative Review. PM & R 2017;9 (5S):S51-58. doi: 10.1016/j.pmrj.2017.02.013.
- Rawstorn JC, et al. Heart 2016;102:1183–1192. doi:10.1136/heartjnl-2015-308966.
- Van Egmond MA et al. Effectiveness of physiotherapy with telerehabilitation in surgical patients: asystematic review and meta-analysis. Physiotherapy. 2018 Sep;104(3):277-298. doi:10.1016/j.physio.2018.04.004.
- Nieman DC, Wentz LM. The compelling link between physical activity and the body’s defense system. J Sport Health Sci 2019;8:201-17. doi: https://doi.org/10.1016/j.jshs.2018.09.009.