By Dr Irfan Ahmed (T: @Irfan_sem)
Over the last week, I have had time to reflect on the twitter feedback from my first blog. I must confess to feeling slightly overwhelmed, the “#softtissuegap” is trending, and has certainly outgrown its initial aim.
One thread debated ‘if SEM should focus on acute care, secondary MSK clinics or even the private sector?’ I have to admit the answers to these questions were not in my initial Plan-Do-Study-Act (PDSA) cycle, but I would welcome the STIM model being adopted in all three!
Planning a new STIM clinic
The initial pitch was simple; I was a new SEM registrar with a bright idea, (I think!). For what we lack in numbers, the SEM community more than makes up for in enthusiasm. Perhaps if we had some evidence-based “soft tissue” pathways, we could amplify our footprint. Take the “Ottawa rules” ankles pathway1, something short and snappy, that could be integrated “up and down” the NHS. In addition to this, the “soft tissue” pathways might help allied health professionals treat & screen patients. The location of the pathway was more accidental than thoughtful, I was based in Emergency Department (ED) at the time. So that’s where the journey began.
Designing a pathway
Our first pathway focussed on “acute knee” injuries, a tricky one where it’s not always easy to identify the injuries that need to be seen. More often than not, the presentation is varied along with the detail of any referral letter. Some patients come armed with a fresh MRI report from the ski slopes, others (less helpfully) a note from the GP detailing a “swollen clicking knee.” Now, if we make the inclusion criteria too broad, we risk being inundated, too tight and we could miss a few. Get it just right though, and our first contact practitioners would be left with something useful and easy to understand.
Improving the patient journey
One retrospective study, (at a typical NHS District General Hospital) revealed that only 14.4%2 of surgically reconstructed ACL injuries were diagnosed at first contact. In addition to this patient consulted a median average of three clinicians2 and waited 13 weeks for the final diagnosis2. All the while hobbling around on an unstable/wobbly knee and risking secondary meniscal tears.
This study made me think surely, we can do better: what if we could reduce the time to diagnosis and number of clinicians seen for acute knee injuries? The sell was a better patient experience and a solution to bridge the “soft tissue gap”.
Fixing the problem however was less clear, often the knee is too swollen to examine on first presentation, and MSK injuries understandably take a lesser priority in the ED. Plus I needed a pathway that worked across the department in the hands of a nurse, paramedic, physiotherapist GP or ED doctor; 365 days a year, 24/7.
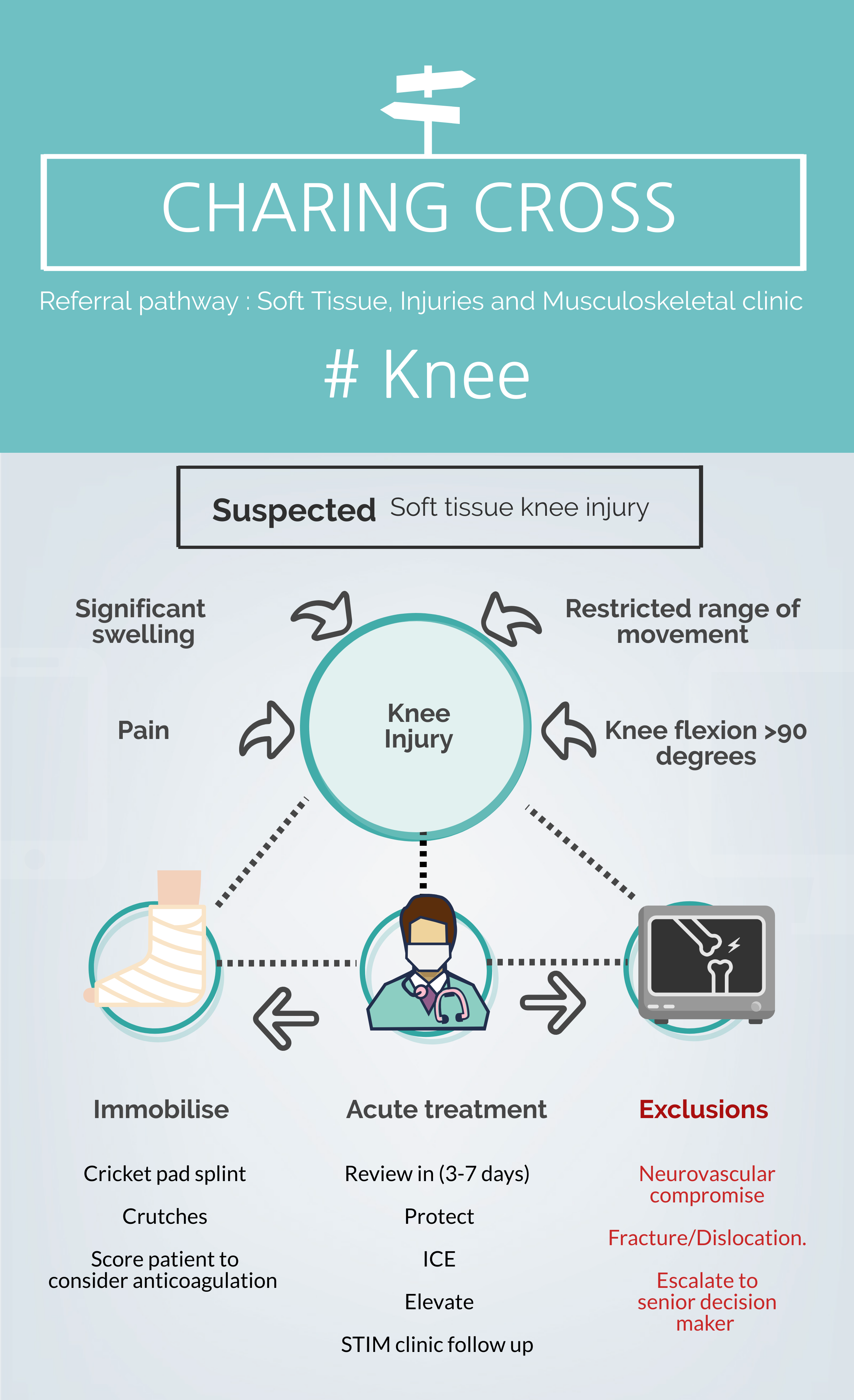
“Charing Cross – Acute Knee Pathway”
In order to overcome some of these challenges, we adopted a standardised “acute knee” pathway (Figure 1). Our theory was simple, early immobilisation, good acute phase management, and when the knee was ripe, bring them back for a diagnostic examination. Once the knee was calm, we could then mentally prepare the patient and get the ball rolling with evidence-based rehab3: quadriceps isometrics exercises, straight leg raises, and establishing a decent range of motion.
Evaluation
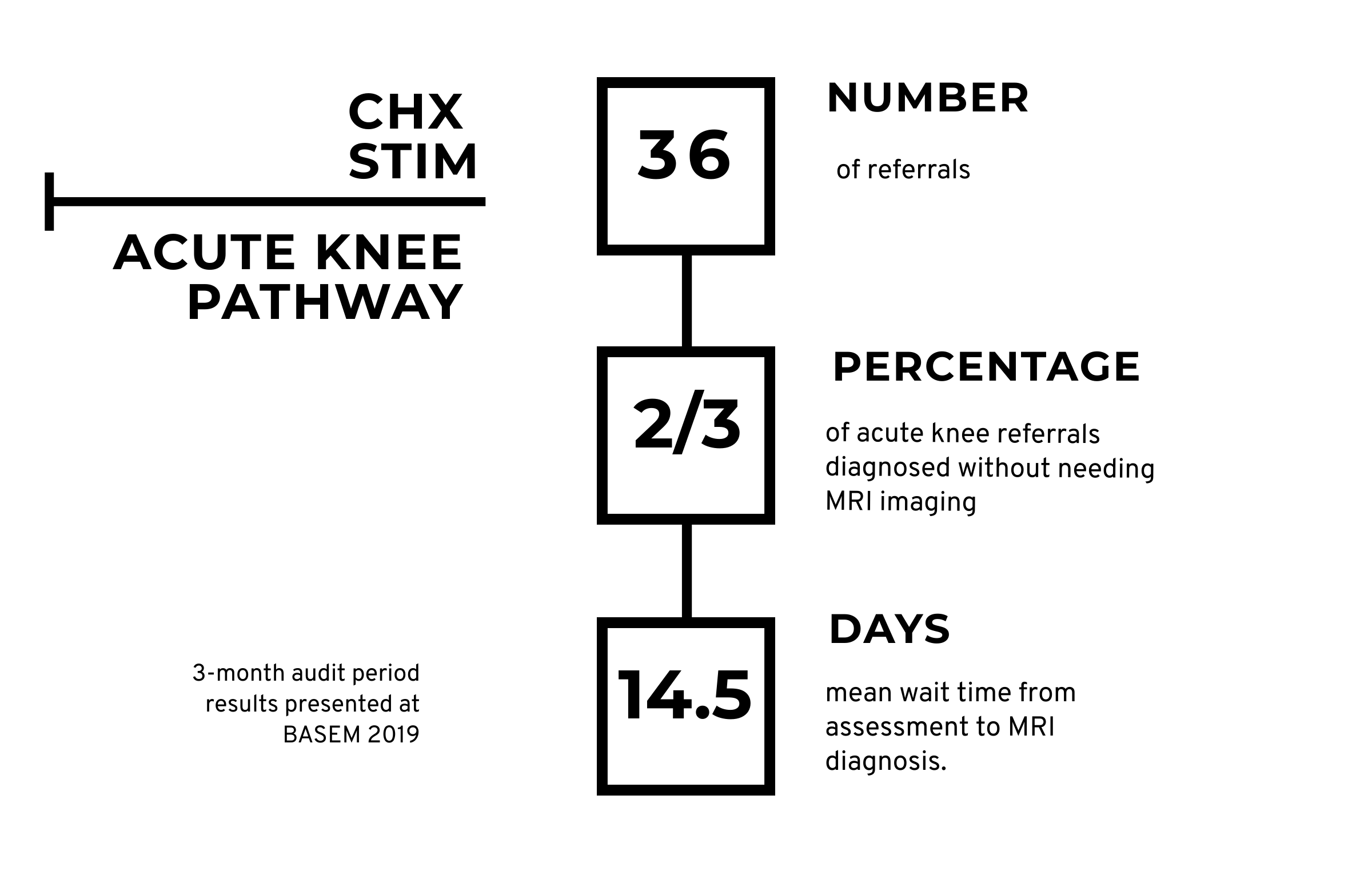
Evaluating a new pathway is always tricky, I mean it depends on who’s paying the bill and who’s making the savings, right? A reduced time to diagnosis (Figure 2), might be enough proof in the world of business; where (time=money) but in an acute NHS trust the lines are often blurred.
Our small pilot has shown financial promise, but even more encouraging for me were the intangibles. Patient satisfaction, engagement with extended scope practitioners and raising the profile of soft tissue injuries in the ED. We hope the “Charing Cross – Acute Knee Pathway” can be adopted in other settings and look forward to publishing data on further pathways later this year.
***
Competing interests
None declared
Dr Irfan Ahmed (T: @Irfan_sem) is a Sport and Exercise Medicine (SEM) registrar (ST4) in London and continues to work as a General Practitioner. Dr Ahmed first developed his interest in SEM at university as a keen amateur boxer and continue to provide match day cover for sporting events. He is involved in teaching, and his current research interest is looking at the impact of mouthguards on athletic performance. Email: irfan.ahmed5@nhs.net
References:
- Bachmann LM, Kolb E, Koller MT, et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ2003:326:417–9
- Parwaiz H, Teo A, Servant C. Anterior cruciate ligament injury: A persistently difficult diagnosis. The Knee. 2016;23(1):116-120
- van Melick N, van Cingel R, Brooijmans F, Neeter C, van Tienen T, Hullegie W et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. British Journal of Sports Medicine. 2016;50(24):1506-1515.