By Kyle A. Winik, Lisa Erasmus and Robyn Paulse
The SASMA conference is a biennial event and the latest instalment – the 17th of its kind – was held in Cape Town. This year’s theme was “Integrate-Accelerate Elevate”. As medical students attending our first conference, we were made to feel extremely welcome and we highly recommend all readers look into attending in 2019! Here are our take home messages!
The Female Athlete: Presenters: Aurelia Natic, Ettie Barsky, Kate Ackerman
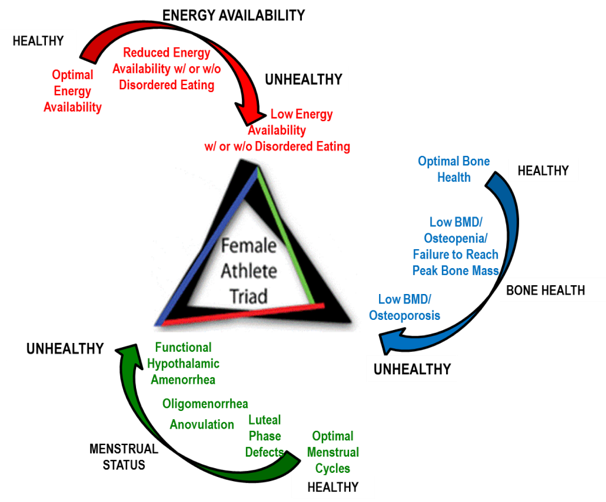
TOP TIP: If ever one component of this triad is positive or worrying, the other two components need to be evaluated.
Optimising bone health is essential early on in life as 90% peak bone mass is achieved by 18 years of age. Another important point was that of identifying fracture risks which can be divided into modifiable and non-modifiable. Modifiable factors contribute 20-40% of the risk and include smoking, drugs, alcohol, hormones, physical activity and nutrition. 60-80% of the risk is attributable to genetics.
http://totalformfitness.com/female-athlete-triad/
Practical tools for implementing the female athlete guidelines:
Evidence-based independent risk factors associated with poor triad outcomes:
- Low energy availability with or without disordered eating/eating disorders
- Low BMI
- Delayed menarche
- Oligo/amenorrhea
- Low BMD
- Stress reaction/fracture history
TOP TIPS for the teenage female athlete. Be alert and look for reasons when:
- BMI <19.5 look for possible issues
- No menarche by 15.5 yo
- 2 or more stress fractures
- Off growth chart
Dr Ettie Barsky also spoke about Exercise in Pregnancy and highlighted that moderate intensity exercise should be done on most if not all days of the week during pregnancy if no medical or obstetric complications are present.
TOP TIP: Target heart rates for age groups 20-29 years and 30-39 years being 145-160bpm and 140-165bpm respectively. A higher fat intake = higher risk of hyperemesis gravidum. Don’t forget danger signs: Ketones, intra-uterine pregnancy, dehydration, over or under weight
Crossing borders to reach our common goals in Sports Medicine: Presenter: Evert Verhagen
Dr Evert Vergahen introduced us to the concept of ‘Crossing borders’ to reach our common goal in sports medicine. He spoke about creating connections with colleagues from all over the world in order to help each other achieve these common goals. The goal being the notion that exercise = medicine but also that as everything in medicine there are adverse effects to be noted and explained to patients.
Optimising the journey of the amputee from surgery to elite performance. Presenter: Jayson Chin, Phoebe Runciman, Wayne Derman.
Another subject that we all found quite interesting but knew very little about was that of the patient with an amputation. From Dr Jayson Chin we learnt that the aim of prosthesis is no longer to get the patient to walk but to provide a good quality of life. Dr Phoebe Runciman also presented a research project comparing mechanical prosthesis and symbionic prosthesis. It was found that with the symbionic prosthesis there were better subjective ratings, 39% improved walking capacity (distance), decreased fatigue with decreased RPE, the rate of loading was lower and it was found that muscle activation patterns and joint angles were closer to normal. We also were shown that we must be aware of genitourinary, skin and subcutaneous illness in para-athletes.
Acute illness in the athlete: Presenters: Martin Schwellnus, Wayne Derman, Alan Kourie, Anri van Tonder, Austin Jeans, Leigh Gordon, Christa Janse van Rensburg, Leslie Bonci.
Acute illness was another subject that we realised was quite important in the athlete. We were made aware that severity of illness is monitored by the time lost and that more than 50% of a team physician’s time is taken up by acute illness treatment. The risk of illness also increases when travelling across more than five time zones and thus a home advantage is key. What most people, including us, would want to know is when the athlete will be fit for return to play after an acute illness and this was answered by Dr Leigh Gordon. We learnt about the ‘neck check’ which states that if the athlete has symptoms above the neck there will be limited return to sport, during this time they will have to do submaximal exercise and should then be re-evaluated. If there are symptoms below the neck or systemic symptoms there should be no sport and should then be re-evaluated at a later stage as complications could arise.
Another component that should be taken into consideration when working with athletes is travel. When travelling to a country the exposures and dangers should be noted by the team physician. Travel in Africa was discussed and three diseases were identified as pertinent: malaria, schistosomiasis and African tick bite fever. Malaria and African tick bite fever can be treated with doxycycline; however, the side effect of photosensitivity should be taken into consideration. Schistosomiasis is treated with praziquantel which is usually safe for athletes.
TOP TIPS:
- Myocarditis is caused by coxsackievirus 50% of the time
- Myopericarditis caused by the influenza virus, can cause the player to be out of practice for 6 months.
- Myoglobin, is significantly increased in pericarditis and is extremely toxic to renal; tubules which could result in renal failure.
- Training with an infection can cause rhabdomyolysis and could result in kidney failure.
- Epstein-Barr virus can cause increased splenic size and subsequently splenic rupture. The athlete should be kept away from non-contact sport for 3 weeks and contact sport for 4 weeks and regular scans should be done to ensure the spleen returns to ‘normal’ size.
- Athletes with Glandular fever should not exercise for 4 weeks and the increase in splenic rupture in males should also be noted.
- Strep throat infection puts the athlete out of training for 1-10 days.
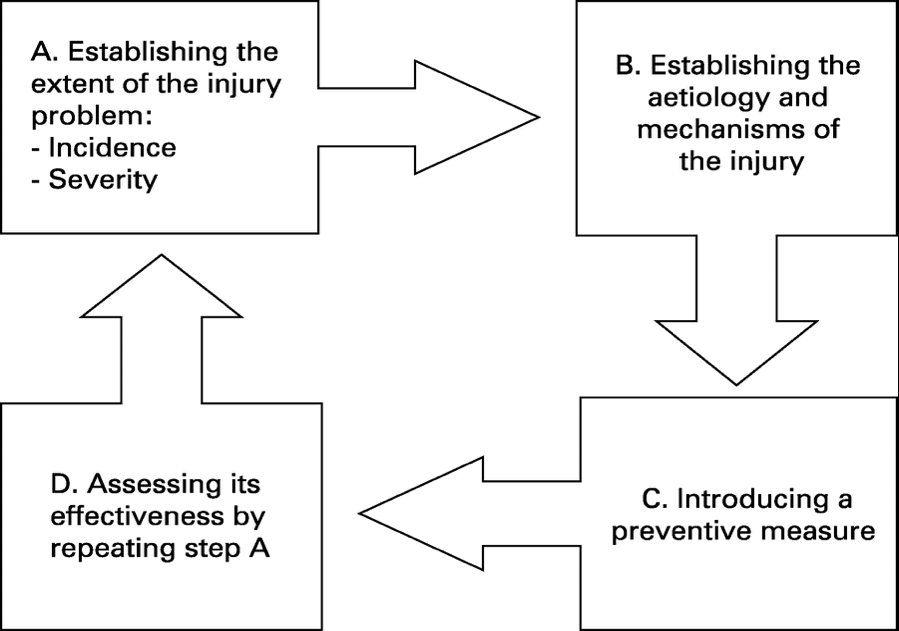
Injury prevention, how far have we come? Presenter: Willem van Mechelen
http://bjsm.bmj.com/content/bjsports/42/8/648/F1.large.jpg?width=800&height=600&carousel=1
TOP TIPS:
- We need to increase the amount of RCTs to assess and evaluate an intervention and its success
- Less than 20% of RCTS in sports injury interventions take compliance into account when measuring outcomes.
Keep your eyes pealed – PART 2 coming soon!
Kyle A. Winik is a 4th year medical student from the University of Pretoria, South Africa. Kyle is extremely passionate about developing his skills in Sport and Exercise Medicine and looks forward to a future profession in the field.