In response to: “Is abdominal hypopressive technique effective in the prevention and treatment of pelvic floor dysfunction? Marketing or evidence from high-quality trials?” (Letter to the editor)
By Saúl Martín Rodríguez @smrodguez and Kari Bø
We thank the authors for the on-going debate about the hypopressive method and its hypothetical benefits on pelvic floor dysfunctions (PFD). The authors start with an introductory paragraph about historical and practical points that, in their opinion, were overlooked in our discussion paper.1 However, the authors should note that what they state about the yoga practices has no evidence and are only historical points that has nothing to do with what we discussed. In fact, we were unable to find any potential level of evidence (systematic reviews with or without meta-analysis or randomized controlled trials, RCT) about the benefits of postural and breathing exercises after the review written by Bø and Herbert2 published in 2013. The above was also stated in our discussion paper and in a recent systematic review.3 Furthermore, it is not true that the bases of PFM exercise dated before Arnold Kegel published his very-well known articles about the exercises that later would take his name.4 Kegel himself actually describes that PFMT has been conducted in other cultures earlier, e.g. in African tribes.
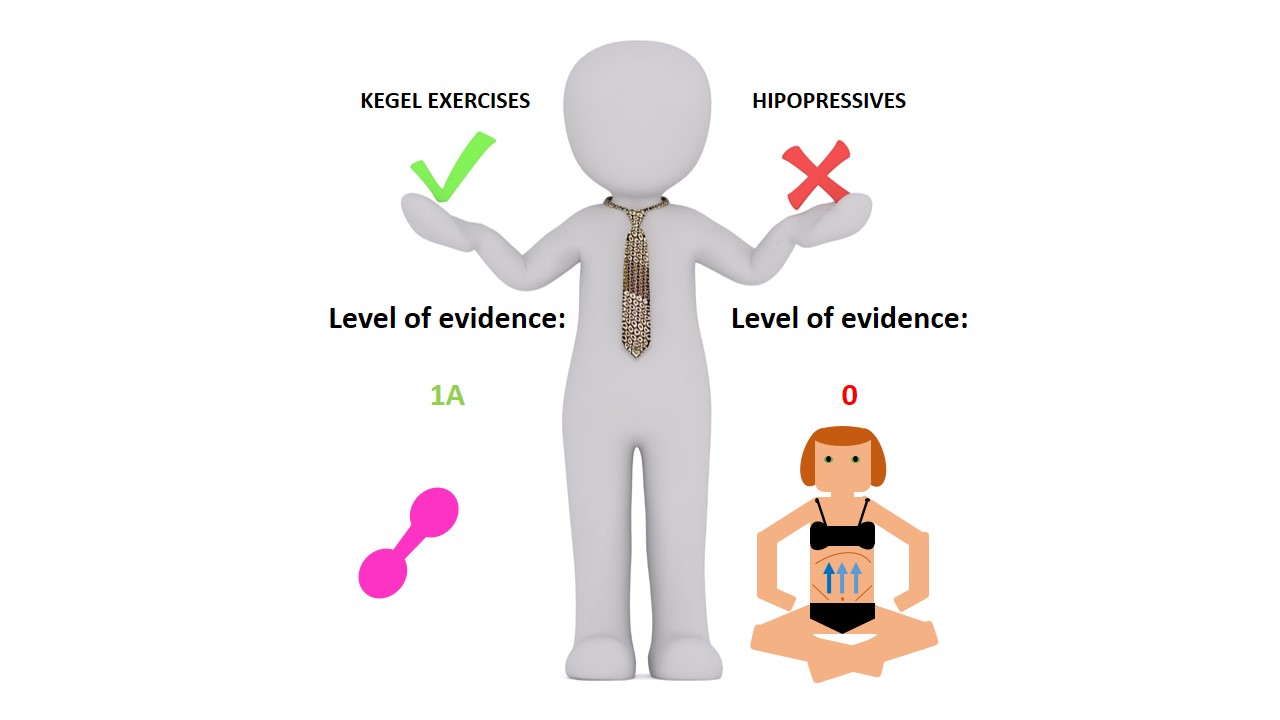
The authors claim that the description of the technical basis we made in our paper of the hypopressive technique was inaccurate. The original description of the technique was defined in 1997 by Caufriez.5 This reference is a book written in French which has been withdrawn and is no longer available or accessible. The description we made was according to the paper of Stupp and colleagues.6 The authors also claim that the description was not according to the public widespread practice or the book written by Rial and Pinsach7. We will argue that the first article published about hypopressive in a journal with quality criteria and indexed, was the publication by Stupp and colleagues.6 Furthermore, we wonder why the authors did not send a letter to the editor at the time discussing if they disagreed about the method used.5 Lastly, we would like to point out that the book of Rial and Pinsach7 is not evidence-based. It only contains multiple speculations. For example, the authors described that the hypopressive technique, besides being useful for PFD, is useful to: regulate metabolic and oxidative factors, preventing any articular and muscular injuries, reducing the abdominal circumference, improving of intestinal activity, or preventing post-natal depression. The above is completely speculative and lacks evidence. As we state in our discussion paper, the above highlights that to date, it is only marketing without strong scientific data to support the supposed benefits (Fig. 1).1
The authors also mention the existence of two observational investigations that show transverse abdominis activation (TrA) and PFM after performing hypopressive exercises. This cannot be used to argue that the technique can prevent and treat urinary incontinence and pelvic organ prolapse. We argue as that you would need blinded RCTs to address such questions.8 In addition, these investigations have been published in journals that do not meet the criteria of scientific rigor and high quality, and hence, are not indexed in the Journal of Citations Reports (JCR). The above is true for the majority of available literature on hypopressive technique that is not indexed in Pubmed and written in a language other than English (i.e., Spanish or French).
Lastly, the authors argue that there is “a growing body of evidence regarding the holistic benefits of postural and breathing exercise programs on health and quality of life”. However, this is again uncertain since Bø and Herbert2 highlighted that breathing and postural exercises are in a development phase. To end, PFMT is inexpensive, easier to learn, and evidence-based. 9,10 In contrast, hypopressives need to be guided by a specialized monitor or physical therapist which implies that they are no longer free or low cost, and they are not, to date, evidence-based. Why change something that already works? Why add something that has no evidence to already proven therapies?
Saúl Martín Rodríguez, is a PhD fellow of the University of Verona (Italy). His research interest include the potential use of exercise combined with drugs in clinical populations. You can follow him on Twitter @smrodguez
Kari Bø, PhD, Professor of the Norwegian School of Sports Sciences (Norway). Her research interest include pelvic floor (function, dysfunction, measurement, prevalence in different groups, prevention, treatment, athletes), women’s health, exercise during pregnancy and after childbirth, low back and pelvic girdle pain, diastasis recti abdominis.
References
- Martin-Rodriguez S, Bo K. Is abdominal hypopressive technique effective in the prevention and treatment of pelvic floor dysfunction? Marketing or evidence from high-quality clinical trials? British journal of sports medicine 2017 doi: 10.1136/bjsports-2017-098046[published Online First: Epub Date]|.
- Bo K, Herbert RD. There is not yet strong evidence that exercise regimens other than pelvic floor muscle training can reduce stress urinary incontinence in women: a systematic review. Journal of physiotherapy 2013;59(3):159-68 doi: 10.1016/s1836-9553(13)70180-2[published Online First: Epub Date]|.
- Ruiz de Vinaspre Hernandez R. Efficacy of hypopressive abdominal gymnastics in rehabilitating the pelvic floor of women: A systematic review. Actas urologicas espanolas 2017 doi: 10.1016/j.acuro.2017.10.004[published Online First: Epub Date]
- Kegel AH. Progressive resistance exercise in the functional restoration of the perineal muscles. American journal of obstetrics and gynecology 1948;56(2):238-48
- Caufriez M. Gymnastique abdominale hypopressive. Bruxelles: M.C. Editions; 1997.
- Stupp L, Resende AP, Petricelli CD, et al. Pelvic floor muscle and transversus abdominis activation in abdominal hypopressive technique through surface electromyography. Neurourology and urodynamics 2011;30(8):1518-21 doi: 10.1002/nau.21151[published Online First: Epub Date]|.
- Rial T, Pinsach P. Hypopressive Techniques: Vigo: Cardeñoso; 2015.
- Burns PB, Rohrich RJ, Chung KC. The Levels of Evidence and their role in Evidence-Based Medicine. Plastic and reconstructive surgery 2011;128(1):305-10 doi: 10.1097/PRS.0b013e318219c171[published Online First: Epub Date]|.
- Dumoulin C, Hay-Smith EJ, Mac Habee-Seguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. The Cochrane database of systematic reviews 2014(5):Cd005654 doi: 10.1002/14651858.CD005654.pub3[published Online First: Epub Date]|.
- Li C, Gong Y, Wang B. The efficacy of pelvic floor muscle training for pelvic organ prolapse: a systematic review and meta-analysis. International urogynecology journal 2016;27(7):981-92 doi: 10.1007/s00192-015-2846-y[published Online First: Epub Date]|.