Implementing black and white guidelines on a grey clinical field.
By Wouter van Everdingen, MD, Prabath Lodewijks, MD, and Tijmen van Assen, MD PhD
Recently the American Heart Association and American College of Cardiology (AHA/ACC) created a combined taskforce to define eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities.1 Recommendations were given for several cardiovascular topics. Albeit comprehensive, the AHA/ACC recommendations on cardiac arrhythmias and conduction abnormalities are quite limiting for a sports physician when used in clinical practice. The recommendations are based on competitive athletes, it is therefore debatable whether they are applicable to recreational athletes. Applying the recommendations to recreational sports might exclude athletes too quickly from all sports-related activities. Moreover, the recommendations lack advice on participation with well-defined limitations. Limitations and alternatives for participation in sports are perhaps beyond the scope of the recommendations, however a sports physician deals with these issues on daily basis. Strict adherence to these guidelines may exclude a large proportion of athletes from healthy physical activity and exercise. A specific set of guidelines for recreational athletes is therefore warranted.
The incidence of events due to cardiovascular disease is relatively low compared the number needed to exclude.2 Athletes with cardiac arrhythmias and conduction abnormalities are therefore specifically suited for sports participation with certain boundaries. These electrophysiological diseases are more ‘grey’ than black and white. As McCartney et al. recently stated on the application of guidelines in clinical practice, these are: “guidelines, not tramlines”.3 Nevertheless, the focus of the recommendations lies on preventing cardiovascular morbidity and mortality caused by extreme conditions of competitive sports. At least the prevention of cardiovascular events is more likely when athletes are excluded. Although the level of evidence on which athletes are excluded is questionable.
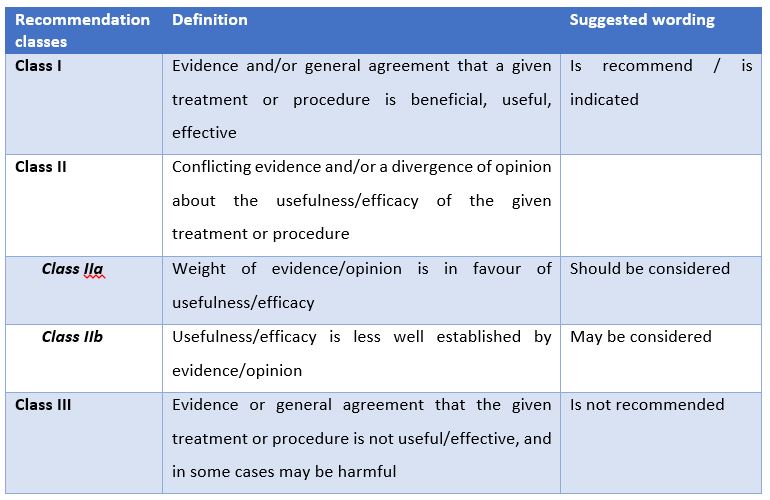
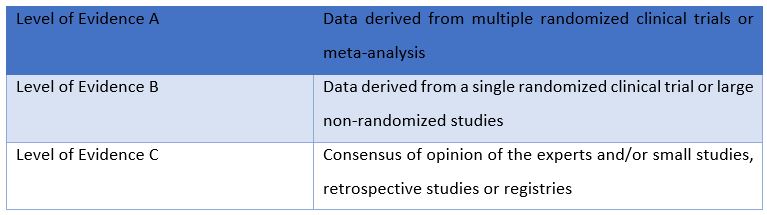
The AHA/ACC statements are mainly accompanied with Class I recommendations, with level of evidence C.1 A class I recommendation may leave no doubt on the matter at hand (table 1). However, doubt is justified when scientific backing is meagre, as level C is the lowest level of evidence (table 2). One might wonder whether ‘consensus of opinion of the experts and/or small studies, retrospective studies, or registries’ justify the highest class of recommendation. Although the percentage of evidence based medicine is improving, sports medicine has much to gain on proper scientific backing.4
In some cases obtaining scientific backing can be difficult, as randomized clinical trials on sports medicine and cardiovascular risks can be unethical. For example, it is relatively unethical to implement randomized clinical trials on the danger of patients with an implantable cardioverter defibrillator (ICD) participating in contact sports. Nevertheless, observational studies on these subjects may be an alternative. There are currently several athletes with an ICD performing in high level activity, such as professional football. Excluding athletes with an ICD may therefore be too restrictive.5 Observational studies can improve acceptance of (recreational) athletes with an implantable cardiac devices (ICD) currently performing in sports. Some surveys already prove the acceptance of ICDs in clinical practice.6 Indeed, approximately 40-60% of electrophysiologists/cardiologists already allow their patients with ICDs to compete. Injury to the athlete or ICD system, reported in a survey, were relatively low (<1% and below 5%, respectively).6 A recent publication by Lampert et al. on athletes with an ICD has already led to a more lenient approach.7 They concluded that athletes with ICDs can participate in competitive sports without health risks despite the occurrence of both inappropriate and appropriate shocks. As stated above, the pros and cons of participation of athletes with an ICD should be weighed on an individual basis.8 The specific sport, level of competition and accompanied dangers should be considered and discussed with the athlete, leading to a patient specific (shared) decision.
Conclusions: can we be more adaptable, inclusive and evidence-based?
The recent statements by the AHH/ACC on eligibility and disqualification of athletes for competitive sports include a thorough set of guidelines. However, these guidelines underscore the absence of an individual approach when implementing guidelines, the absence of guidelines for recreational athletes, and the problem of applying consensus opinion without adequate evidence as a Class I recommendation. Moreover, these guidelines indicate a gap in the evidence based approach in treating cardiovascular diseases in sports medicine. While this might seem a drawback, it offers a wide field of opportunities for future research. A careful and open minded approach is advised to prevent (recreational) athletes sitting at home, possibly succumbing to the negative effects of inactivity.
References
- Zipes DP, Link MS, Ackerman MJ, Kovacs RJ, Myerburg RJ, Estes NA, 3rd. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 9: Arrhythmias and Conduction Defects: A Scientific Statement From the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015;66:2412-23.
- Bessem B, Groot FP, Nieuwland W. The Lausanne recommendations: a Dutch experience. Br J Sports Med 2009;43:708-15.
- McCartney M, Treadwell J, Maskrey N, Lehman R. Making evidence based medicine work for individual patients. BMJ 2016;353:i2452.
- Grant HM, Tjoumakaris FP, Maltenfort MG, Freedman KB. Levels of Evidence in the Clinical Sports Medicine Literature: Are We Getting Better Over Time? Am J Sports Med 2014;42:1738-42.
- Heidbuchel H, Carre F. Exercise and competitive sports in patients with an implantable cardioverter-defibrillator. Eur Heart J 2014;35:3097-102.
- Lampert R, Cannom D, Olshansky B. Safety of sports participation in patients with implantable cardioverter defibrillators: a survey of heart rhythm society members. J Cardiovasc Electrophysiol 2006;17:11-5.
- Lampert R, Olshansky B, Heidbuchel H, et al. Safety of sports for athletes with implantable cardioverter-defibrillators: results of a prospective, multinational registry. Circulation 2013;127:2021-30.
- Lampert R, Cannom D. Sports participation for athletes with implantable cardioverter-defibrillators should be an individualized risk-benefit decision. Heart Rhythm 2008;5:861-3.
Tables
Table 2. Levels of evidence
| Level of Evidence A | Data derived from multiple randomized clinical trials or meta-analysis |
| Level of Evidence B | Data derived from a single randomized clinical trial or large non-randomized studies |
| Level of Evidence C | Consensus of opinion of the experts and/or small studies, retrospective studies or registries |
Bio’s
Wouter van Everdingen, MD, is resident in sports medicine and PhD-student at the department of cardiology, both in the University Medical Centre (UMC) Utrecht, Utrecht, The Netherlands. As an amateur endurance athlete, he is enthusiastic on aiding competitive and recreational athletes in the department of sports medicine in Utrecht. His research at the department of cardiology focusses on electrophysiology, specifically the optimization of cardiac resynchronisation therapy.
Prabath Lodewijks, MD, is a sports physician in the University Medical Centre (UMC) in Utrecht. He is also the team physician of FC Utrecht, a professional football team playing in the Dutch Eredivisie, the highest league of The Netherlands.
Tijmen van Assen, MD PhD is a resident in sports medicine at the University Medical Centre (UMC) in Utrecht. Before the start of his residency, he conducted his PhD studies on the Anterior Cutaneous Nerve Entrapment Syndrome (ACNES).