LETTER TO THE EDITOR
In response to:
Dear Editor,
Recently a systematic review was published in your journal by de Vos et al (1) on the effect of PRP (Platelet rich plasma) injections in the treatment of chronic lateral epicondylar tendinopathy. They conclude there is strong evidence that PRP injections are not efficacious in the management of chronic lateral epicondylitis (LE).
In our opinion the conclusions drawn in this study are too firm and not properly supported by recent literature. In the review, PRP injections are compared to different other injection therapies as control group. In three of the included studies PRP injections are compared to corticosteroid injections (2,4,7). In current literature and stated by the authors of current review there are several studies that demonstrate a short term (4- 6 weeks) beneficial effect of glucocorticoid injections on pain in the treatment of lateral epicondylitis (11,12,13,14). The review by Krogh et al (11) found no long term benefits of glucocorticoid injection over placebo. After 12 months, conservative treatment appears more effective: 8 till 9 of 10 patients are pain free versus 7 of 10 patients having had corticosteroids. Therefore it cannot be used as a control group to investigate the efficacy of PRP injections, in fact it is even not ethical to use these as a comparison in future trials. The follow up of the study by Omar et al (7) was only 1.5 months. This may explain why there were no differences in outcome measures between the PRP and the corticosteroid group. The meta-analysis by Krogh et al (11) also showed that autologous blood, PRP, prolotherapy and hyaluronic acid were all more efficacious than placebo in the treatment of LE.
A relevant question in the discussion about the treatment of LE with injection therapies is the difference in effectiveness between PRP and autologous whole blood. The included study by Thanasas et al (5) shows a trend of decreasing VAS scores in favor of the PRP group (VAS improvement of 4.4 points (71%) compared to mean VAS improvement 3.4 points (58%)), no significant differences are found. The study by Creaney et al (6) showed no difference in VAS scores between PRP and autologous whole blood.
Because a meta-analysis has the highest level of evidence we performed a systematic search in Pubmed/Medline to identify trials comparing PRP with ABI in the treatment of LE. Four publications were identified (5,6,9,10). This first meta-analysis should be updated in the future to summarize the most up to date evidence.
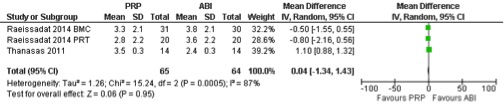
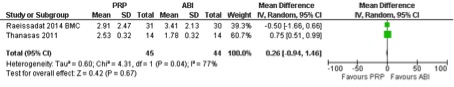
To support these findings we have pooled data of the study by Thanasas et al (5) and data of recent studies on the effect of Platelet-rich plasma versus autologous whole blood for the treatment of LE by Raeissadat et al (9, 10). This shows no differences in VAS painscores after six weeks (table 1) and 6 months (table 2) after treatment with PRP or autologous whole blood. Standard Deviations (SD) are estimated based on ranges or 95 % confidence intervals.
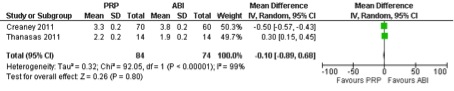
Creaney et al (6) and Thanasas et al (5) both used a (different) functional outcome score. Data of the two studies were pooled and showed no differences in functional improvement between PRP and autologous whole blood (table 3).
It is possible that the two studies by Raeissadat and colleagues (9, 10) used the same dataset, given the overlap in inclusion period. If this is the case, it would perhaps be better to consider them as one study. Due to the high level of heterogeneity, no firm conclusion can be drawn. Nevertheless, it is questionable to what extend there is a relevant difference in the treatment effect between PRP versus whole blood. When there is no difference in treatment effect, treatment with autologous whole blood is preferred due to the higher costs of preparation of PRP.
To answer this question, a high quality study is needed to compare the effects of autologous whole blood with PRP and placebo in the treatment of LE. In current literature the injections therapies are performed manually and blindly and are therefore not properly comparable (11). Future studies should be performed in a standardized way by an ultrasound guided reproducible and well defined injection technique to make the interventions comparable.
Sincerely,
Renee Keijsers
Denise Eygendaal
Michel P. J. van den Bekerom
References
- de Vos, R-J, Windt J, Weir A. Strong evidence against platelet-rich plasma injections for chronic lateral epicondylar tendinopathy: a systematic reviewBr J Sports Med doi:10.1136/bjsports-2013-093281.
- Peerbooms JC, Sluimer J, Bruijn DJ, et al. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: platelet-rich plasma versus corticosteroid injection with a 1-year follow-up. Am J Sports Med 2010;38:255–62.
- Gosens T, Peerbooms JC, van Laar W, et al. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: a double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med 2011;39:1200–8.
- Krogh TP, Fredberg U, Stengaard-Pedersen K, et al. Treatment of lateral epicondylitis with platelet-rich plasma, glucocorticoid, or saline: a randomized, double-blind, placebo-controlled trial. Am J Sports Med 2013;41:625–35.
- Thanasas C, Papadimitriou G, Charalambidis C, et al. Platelet-rich plasma versus autologous whole blood for the treatment of chronic lateral elbow epicondylitis: a randomized controlled clinical trial. Am J Sports Med 2011;39:2130–4.
- Creaney L, Wallace A, Curtis M, et al. Growth factor-based therapies provide additional benefit beyond physical therapy in resistant elbow tendinopathy: a prospective, single-blind, randomised trial of autologous blood injections versus platelet-rich plasma injections. Br J Sports Med 2011;45:966–71.
- Omar AS, Ibrahim ME, Ahmed AS, et al. Local injection of autologous platelet rich plasma and corticosteroid in treatment of lateral epicondylitis and plantar fasciitis: randomized clinical trial. Egypt Rheumatol 2012;34:43–9.
- Mishra AK, Skrepnik NV, Edwards SG, et al. Platelet-rich plasma significantly improves clinical outcomes in patients with chronic tennis elbow: a double-blind, prospective, multicenter, controlled trial of 230 patients. Am J Sports Med 2014;42:463–71.
- Raeissadat SA, Rayegani SM, Hassanabadi H, Rahimi R, Sedighipour L, Rostami K. Is Platelet-rich plasma superior to whole blood in the management of chronic tennis elbow: one year randomized clinical trial. BMC Sports Sci Med Rehabil. 2014 Mar 18;6(1):12.
- Raeissadat SA, Sedighipour L, Rayegani SM, Bahrami MH, Bayat M, Rahimi R. Effect of Platelet-Rich Plasma (PRP) versus Autologous Whole Blood on Pain and Function improvement in Tennis Elbow: A Randomized Clinical Trial. Pain Res Treat. 2014;2014:191525. doi: 10.1155/2014/191525. Epub 2014 Jan 20.
- Krogh TP, Bartels EM, Ellingsen T, Stengaard-Pedersen K, Buchbinder R, Fredberg U, Bliddal H, Christensen R. Comparative Effectiveness of Injection Therapies in Lateral Epicondylitis: A Systematic Review and Network Meta-analysis of Randomized Controlled Trials. Am J Sports Med 2013 Jun;41(6):1435-46.
- Gaujoux-Viala C, Dougados M, Gossec L. Efficacy and safety of steroid injections for shoulder and elbow tendonitis: a meta-analysis of randomised controlled trials. Ann Rheum Dis. 2009 Dec;68(12):1843-9. Epub 2008 Dec 3.
- Hay EM, Paterson SM, Lewis M, Hosie G, Croft P. Pragmatic randomised controlled trial of local corticosteroid injection and naproxen for treatment of lateral epicondylitis of elbow in primary care. BMJ. 1999;319:964-968.
- Smidt N, Lewis M, Van der Windt DA, Hay EM, Bouter LM, Croft P. Lateral epicondylitis in general practice: course and prognostic indicators of outcome. J Rheumatol. 2006;33:2053-2059.