Article originally published in the Aspetar Sports Medicine Journal as part of a Targeted Issue on Post-Exercise Recovery and is reproduced with the kind permission of Aspetar – Orthopaedic and Sports Medicine Hospital.
By Christophe Hausswirth, France
Elite athletes often train intensitively or compete over consecutive days. Cumulative fatigue over such periods of training or competition can reduce athletic performance. Adequate recovery between training sessions and/or competitive events is therefore essential to minimise the risk of fatigue and optimise performance. In this context, the use of whole-body cryotherapy (WBC) as a tool to aid recovery shows benefits on some inflammatory parameters, possible improvement of antioxidant status and improvements in mood and mild depression. Heating the body is supposed to be beneficial to athletes’ recovery, to treat muscle pain and as part of rehabilitation after injury. It has been already demonstrated that WBC stimulates the physiological reactions of an organism which results in analgesic, anti-swelling, antalgic immune and circulatory system reactions and could improve recovery after muscular trauma injury. Definition is needed as to the precise context in which athletes may use this tool to optimise recovery in relation to improving sleep patterns, optimising the parasympathetic system and increasing their general well-being.
INTRODUCTION
Exercise-related stress is often increased due to environmental conditions, particularly those relating to temperature changes. For every sporting activity there is an ideal ambient temperature. Any deviation from this reference temperature will have a negative impact on performance.
Indeed, physical activity in a warm or cold atmosphere means that the body and the mechanisms involved in temperature regulation have to work harder. Although very effective, these thermoregulatory mechanisms may not be able to cope with extreme conditions.
They do, however, allow the body to adapt during chronic exposure. Artificial cooling of ambient temperature is an evolving technique, both to prepare athletes for competitions in difficult conditions and to improve the body’s recovery capacity.
HISTORICAL BACKGROUND FOR WHOLE-BODY CRYOSTIMULATION
The first very low temperature cold rooms appeared in Japan in 1989, when Yamauchi used a cryogenic chamber to treat rheumatism. The indications for WBC were subsequently extended to various inflammatory conditions. WBC was then offered to treat pain and prevent post-traumatic oedema, with exposure limited to to 2 to 3 minutes.
One of the most well-established physiological responses to cold exposure is triggered by the decrease in skin temperature, promptly stimulating cutaneous receptors and their sensory afferents to excite sympathetic adrenergic fibres, in turn causing the constriction of local arterioles and venules. The resulting decrease in blood flow to the periphery or injured/inflammed tissues reduces local metabolic processes, thereby attenuating the inflammatory response and the formation of oedema around the injured tissues1.
Reported reasons for using WBC include decreased joint pain and disorders, improved general well-being, decreased fatigue perception2 and reduced symptoms of psychiatric disorders such as anxiety and depression3. WBC is also extensively used in self-treatment or body hardening against respiratory tract infections and musculoskeletal pain4, as well as parasympathetic reactivation after intensive exercise5.
COLD ENVIRONMENT: THE CASE FOR WHOLE-BODY CRYOSTIMULATION-CRYOTHERAPY
What is known today: a review of scientific data
How well WBC restores biological constants following intensive training remains unclear. Studies are therefore ongoing in the field of athlete recovery.
Although we still lack scientific hindsight on the link between recovery, sport and cryostimulation, this paper will summarise the effects of WBC on some relevant parameters and practical applications from our point of view. This will help to identify possible applications in the field of recovery in sport. The first parameter subjected to in-depth studies was inflammation; some studies associate recovery with the kinetics of appearance of inflammatory and/or muscle injury markers. At INSEP (French National Institute of Sport, Expertise and Perfomrance) we have been working for 4 years to help both the medical and the performance-related recovery process.
Sport and cold exposure
In the sporting realm, WBC (in this instance, more accurately defined as whole-body cryostimulation) has been used at temperatures ranging from -110°C to -160°C with the aim of limiting the spread of muscle lesions after training or competing6. It has also been offered as a prophylactic treatment to reduce the risk of muscle lesions during intense training periods and to increase the antioxidant status after multiple exposures7. Despite the increasing popularity of WBC in sports, few studies have assessed its efficacy in accelerating the recovery of the athlete2,8. Very recently, post-exercise cold water immersion has been shown to aid recovery by altering blood flow9, and improving perceptions of recovery10 which may be reflected by changes in cardiac autonomic activity. WBC may also exert important effects on post-exercise recovery at the cardiovascular level. As exercise causes an intensity-dependent parasympathetic withdrawal and sympathetic increase, a prompt recovery of parasympathetic activity is desirable after exercise. Changes in cardiac parasympathetic activity as assessed by heart rate variability (HRV) analysis have emerged in the literature as a global recovery index that reflects the acute response of the body to exercise; an elevated level of parasympathetic activity allows rapid cardiodeceleration and faster recovery10,11. While Stanley et al10 demonstrated that both cold water immersion (5 minutes in 14°C water) and contrast water therapy, consisting of three cycles alternating immersion in cold (1 minute, 14.2°C) and warm (2 minutes, 35.5°C) water, significantly aided post-exercise parasympathetic reactivation compared to passive recovery (PAS) in trained endurance athletes, they also reported that this effect was larger with cold water immersion than contrast water therapy, suggesting that combining a greater cold stimulus increased the effectiveness of water immersion. While various water immersion protocols have been shown to accelerate post-exercise parasympathetic reactivation, the effect of dry air whole-body cryostimulation (range from -110°C to -160°C) on post-exercise autonomic recovery is not well-documented, even though this recovery method has become increasingly used in high level sport3,8. Only one study reported a significant increase in the HRV indices of parasympathetic activity following a WBC session performed after exercise in elite synchronised swimmers5. Similarly, in resting conditions, Westerlund et al12 found that a single session of WBC significantly augmented HRV indices of parasympathetic modulation in healthy non-athletic women, with a mean increase of approximately 50% in root mean square of the successive differences and high frequency power. The resulting increase in central pressure in turn activates the baroreflex, responsible for reducing sympathetic nerve activity while shifting autonomic heart rate control toward a parasympathetic dominance. However, in the case of healthy, recreationally active men training only a few times per month, the autonomic response to WBC has not been investigated. Further, the influence of WBC on blood parameters and subsequent cardiac and thermal responses compared to partial-body cryostimulation (PBC) technique has not been thoroughly evaluated.
Comparison in different techniques of cold stimulation
Modern cryotherapy techniques involve local, partial-body and whole-body exposures. WBC and PBC have been developed very recently and many devices are commercially available. The major differences in the two systems are:
- the temperatures (-110°C vs -160°C for WBC and PBC, respectively),
- whether the head is exposed to the cold stimulus (yes vs no for WBC and PBC, respectively),
- the source of cold stimulation (compressor vs nitrogen gas for WBC and PBC, respectively).
The infrared studies of the temperature response to 3 minutes WBC exposure reported that cold air on the entire human body was responsible for an obvious drop off in skin temperature whereas central temperature did not exceed the thermoregulation range during cryotherapy sessions13. Thermal mapping of the body could be influenced by local blood flow, degenerative and inflammatory state of the tissue. It was therefore previously reported that an enhancement of skin temperature profile could increase the diagnostic sensitivity of infrared imaging in patients13. The use of several types of cryostimulation raises new questions such as:
- What is the optimal modality?
- What are the duration and minimal temperature required to elicit physiological responses?
- Is head exposure needed to induce general modifications?
During WBC the entire body is exposed to cold, including the face and neck, as opposed to a PBC session. It has been shown that the direct effect of cold on the head alone, via face immersion in cold water (without breath holding) aided parasympathetic reactivation significantly following exercise11. The results of a recent study conducted at INSEP showed that whatever the cryotherapy technique used, a single 3-minute cryostimulation induced a strong autonomic response, as rising plasma noradrenaline, systolic and diastolic blood pressures reflected increased sympathetic activation and as the rise in HRV indices suggested an augmentation of the parasympathetic control of heart rate. A likely greater parasympathetic activation was observed with the greatest body cooling obtained by exposing the whole body (WBC) to cold.
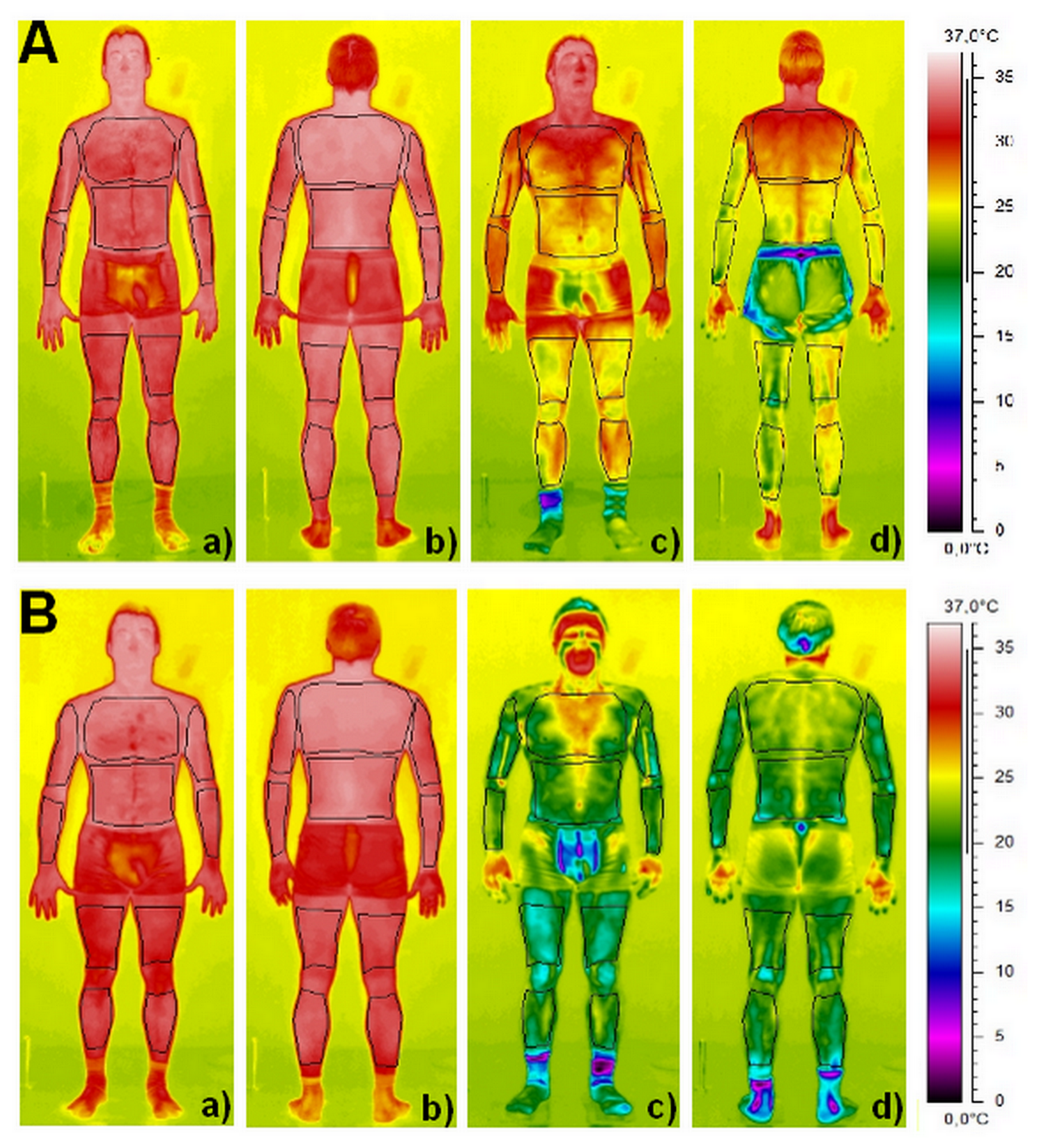
Contrary to localised cryotherapy obtained by the application of ice packs, cold towels or cold air-pulsed on a small body region, the air-based cryotherapy modalities examined in the present study14 involved either complete body cooling (WBC) or whole-body cooling except the head and neck (PBC), inducing an important decrease in whole-body temperature (Figure 1). An almost certain very large reduction in Tskin (skin temperature) of all body regions of interests was recorded after the 3-minute cryostimulation, in greater proportion with the WBC. The mean decrease in Tskin was 13.7°C (i.e. -42.9%) for WBC and 8.3°C (i.e. -26.1%) for PBC. As previously reported by Cholewka et al13, a larger decrease in Tskin was recorded in the legs and arms when compared with the torso and back (Figure 1). These authors reported a significant positive correlation between the decrease in Tskin and the body mass index of individuals, indicating that the effects of cryostimulation may be influenced by body composition.
Cold-related stimulation of the autonomic nervous system
Hear Rate Variability (HRV) indices and blood catecholamines are classically used to evaluate the modulation of the autonomic nervous system (ANS) in response to various stimuli such as cold or physical exercise5,11. The parasympathetic and sympathetic activities refer to the cholinergic and adrenergic phases of the ANS, in reference to their respective neurotransmitters (i.e. acetylcholine for the parasympathetic component and catecholamines for the sympathetic component). Given the lack of consensus on the accuracy of HRV analysis in assessing sympathetic activity, we stated that the activity of this component of the ANS was studied only through plasma catecholamine concentrations, while the parasympathetic component was studied through HRV analyses. Plasma noradrenaline concentrations were likely and very likely increased after the PBC and WBC sessions, respectively, suggesting increased sympathetic nerve stimulation. This increase in plasma noradrenaline was accompanied by a possible small increase in plasma dopamine after WBC only, but no response in plasma adrenalinewas recorded after PBC and WBC sessions. Similar findings (cold-induced increases in plasma noradrenaline without any changes in plasma adrenaline) have been reported after different modalities of cold exposure15. Since noradrenaline mostly originates from the sympathetic nerve endings and adrenaline from the adrenal medulla, we can suggest that both cryostimulation techniques activate the sympathetic nerve system. In addition, since an increase in plasma dopamine is typically related to sensations of well-being and pleasure, we can suggest a slightly greater effect of WBC in generating positive feelings. A previous study reported a significant increase in sensations of well-being when an exhaustive treadmill running protocol was followed by a WBC session2.
During cryostimulation, cold-sensitive cutaneous receptors excite the sympathetic α-adrenergic fibres, responsible for a peripheral vasoconstriction mechanism through the release of noradrenaline. Consequently, blood flow is redistributed toward the core, resulting in increased arterial pressure16. INSEP data suggested that systolic and diastolic blood pressure were very likely increased after WBC, but not after PBC, pointing to a lower sympathetic stimulation that may be related to the smaller decrease in Tskin obtained after PBC. Further, the decrease in Ttymp (tympanic temperature )recorded with WBC, as well as the stimulation of cold trigemino-cardiac reflex receptors located in the face may have accentuated the parasympathetic response after WBC, augmenting vagal output to the heart. As expected, the increase in blood pressure was associated with a large decrease in heart rate, that was larger after WBC (-15.2%) than PBC (-10.9%) likely reinforced by the concomitant triggering of the baroreflex which lowers the sympathetic tone of the ANS, shifting to a predominance of the parasympathetic tone.
We published recently published a paper of the effect of WBC single exposure on recovery in elite athletes5. To our knowledge, this is the first time that WBC was investigated as a recovery technique between two closely scheduled, sport-specific maximal exercise bouts. The two most important findings of this study were:
- using WBC shortly after a full-length synchronised swimming ballet resulted in a strong parasympathetic reactivation in elite swimmers, yielding two- to four-fold increases in vagal-related HRV indices compared to pre-exercise values within only 1 hour;
- WBC exerted a significant influence on metabolic parameters of recovery and subsequent exercise, with a larger clearance of plasma lactate and an increase in maximal aerobic work output during the second ballet. The latter was only matched by the effects of active recovery.
Inflammatory marker responses
Some authors have measured various markers of inflammation in subjects exposed to very low temperatures. Banfi et al7 showed that treating top-level rugby players with WBC for 1 week led to reduced rates of pro-inflammatory cytokines (IL-2 and IL-8) and increased levels of anti-inflammatory cytokines (IL-10). This is the only study in which the results can genuinely be related to recovery after intense muscular exercise. According to the authors, WBC should improve muscle recovery, although they were not able to measure to what extent.
In this 5-day study, 10 top-level rugby players were placed in cryogenic chambers at -60 C for 30 seconds, then at -110 °C for 120 seconds. In addition, subjects followed their normal 3-hour daily training without changing their workload. While no significant difference was measured in terms of immunoglobulin or C-reactive protein levels (two markers of acute inflammation), the authors did show that creatine kinase and PGE2 prostaglandin concentrations were significantly reduced after 5 days of WBC (Figure 2). No control group was included in this study. The authors explain that the drop in creatine kinase is likely to result from the stimulation of noradrenalin secretion during exposure to cold, an effect demonstrated in Rønsen et al’s18 study. No assay of noradrenalin was performed in this study.
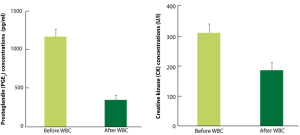
Banfi et al17 observed a reduction in PGE2 associated with reduced creatine kinase levels. PGE2 is synthesised at the site of inflammation, where it acts as a vasodilator in synergy with other mediators, such as histamine and bradykinin. These mediators cause increased vascular permeability leading to oedema. Their reduction, after 5 days of WBC, seems to be a good indicator of improved muscle recovery. However, the absence of a control group in the study is a flaw which makes it impossible to reliably conclude on the efficacy of WBC in recovery. This research does, however, offer some suggestions as to the parameters likely to favour (or not) improved recovery.
In a recent study8 conducted in order to analyse the effect of two different recovery modalities on classical markers of exercise-induced muscle damage and inflammation obtained after a simulated trail running race. We chose to compare changes in immune cell mobilisation and C-reactive protein level because they are reliable indicators of acute performance deterioration, muscle damage and/or inflammation routinely evaluated in the general population and in athletes4,9. The major finding was that a single exposure to WBC significantly alleviated inflammation after strenuous exercise.
- Delta IL-1ra increased 1 hour after exercise following WBC compared to PAS
- Delta IL-1β was significantly suppressed 1 hour after exercise following WBC, compared to the PAS condition,
- WBC minimised the decrease of neutrophils 24 hours after exercise and
- C-reactive protein increase was strongly limited in the WBC group compared to the PAS group at 24 hours and until 48 hours after exercise. Data confirm that the treatment induces an anti-inflammatory protection effect and suggest that WBC reduced the time of recovery by positive effects on immunological parameters and the regeneration process for elite athletes.
Hormonal responses
Most studies of WBC have focused on the kinetics of biochemical markers and/or how various hormones evolve in response to exposure. It is widely believed that changes (or lack of changes) to endocrine parameters are relevant topics for research on improved athlete recovery. In this context, a recent study by Smolander et al19 compared WBC exposure (-110 °C for 2 minutes) to cold-water immersion (0-2 °C for 20 seconds). The two groups were subjected to either treatment weekly over a total of 12 weeks. Various hormones – growth hormone, prolactin and the thyroid hormones (TSH, T3, T4) – were analysed. The authors concluded that there were no significant variations in hormone levels for the WBC group. Prolonged exposure to cold seems to have no effect on the concentrations of these hormones. Based on this lack of effect of WBC on hormone levels, we can conclude that this procedure conforms to sporting ethics. These results are supported by those of another recent study by Banfi et al17, who indicated that, for a group of 10 athletes, none of the haematological parameters (e.g. red blood cells, white blood cells, haematocrit, haemoglobin, platelets etc.) were affected by five 2-minute exposures over 1 week. In an earlier study, Leppäluoto et al15 showed that exposure to WBC (three times per week for 12 weeks) induced a significant increase in plasma noradrenalin levels (Figure 3). The authors explain that the increases in noradrenalin levels recorded over the twelve weeks could play a role in relieving perceived pain, an effect seen in other studies using traumatising exercise. However, no scale of pain perception was offered in this purely descriptive study, which involved straightforward cryostimulation by WBC exposure.

Immune responses
For a number of years, the immune system has been of particular interest to sports physiologists. The incidence of sore throats in very fit athletes initially helped doctors to detect overtraining syndrome. These intuitions were confirmed more recently by some very well-run American and UK studies.
In this context, Nieman20 observed that the immune response was impaired during repeated phases of prolonged high-intensity exercise, and that athletes responded poorly to bacterial and viral attacks, thus delaying recovery. Excessive sensitivity to respiratory tract infections seems to set in gradually, although it is well-described that the risk of respiratory infection follows a ‘J-shaped’ curve when plotted against training intensity, and that moderate exercise results in a low risk. Training is known to improve the immune response to a certain degree, while overworked athletes have reduced immune responses, in particular for immunoglobulins, ‘Natural Killer’ or ‘NK’ lymphocyte subgroups. While no study deals with the kinetics of how the immune system evolves after exposure to WBC, mainly because the procedure is so new, models involving swimming and immersion in cold water have been used for the last few years in Nordic countries and have provided indications on how the immune system is affected. This practice, which was developed more on a cultural than on a scientific basis, has always been empirically linked to improved resistance to infections. In this context, Dugué and Leppänen21 showed, in a study comparing populations swimming regularly in cold water or not, that plasma IL-6 levels, monocytes and leukocytes were all higher in cold-water swimmers. The authors concluded that the immune system of cold-water swimmers was controlling the inflammatory response better and that repeated exposure to cold (by immersion or not) could explain the improvement in defence against infections. It could therefore be suggested that repeated exposure in cold rooms (i.e. WBC) stimulates the immune system and reduces susceptibility to infections in acclimatised individuals. New studies on WBC should shed light on these hypotheses and offer insights into the relationships between immunity, cold and athlete recovery.
Antioxidant status responses
Physical exercise is known to be characterised by an increase in oxygen consumption, and consuming high levels of oxygen is associated with increased free radical production. Modulation of oxygenated free radical production plays a clear role in muscle recovery after exercise. High intensity exercise and/or exercise involving many eccentric movements are a true stress, producing metabolic by-products with significant effects on cellular structures. Oxygen-derived free radical species involved in oxidative stress are of various structures, but all are extremely reactive compounds which, once produced, will oxidise various cellular components. This oxidation can lead to cellular dysfunction and, among other things, to inflammatory disorders. A recent study by Dugué et al22 showed increased total plasma antioxidant capacity after 36 cold room sessions over 12 weeks (three times per week). These results contradict the authors’ initial hypothesis that values would be significantly reduced, and explain the improved protection. A single study investigated the effects of a WBC session (at -130°C) on the pro-oxidant/antioxidant ratio7. Plasma total oxidant status was significantly lower 30 minutes after exposure to WBC for 3 minutes (Figure 4). The next day, the total oxidant status level was still significantly lower compared to the basal level before WBC exposure. In addition, total antioxidant status values were significantly lower 30 minutes after exposure to cold, but did not differ from basal values the next day. However, in the case of athletes, cryostimulation is combined with physical exercises as part of regular training, and it is therefore difficult to know to what extent lipid peroxidation is the result of training and/or cryostimulation6.

Responses for depressive symptoms
Some studies investigated the somatic and psychological effects of cold and seemed to reach a consensus on mood alterations. Even if somatic and psychological parameters seem somewhat removed from the topic of recovery in sport, they can obviously play an indirect role. Thus, the first studies on the subject showed that a short exposure to WBC improved sleep, sense of relaxation and mood, and that these effects can persist for hours or even days. In a more recent study, Rymaszewska et al3 studied the effects of WBC (-150 °C, 160 seconds, 10 times over 2 weeks) in 23 depressed patients on anti-depressant treatment. Using the 21 items on the ‘Hamilton Rating Scale for Depression’ (HRSD), the authors concluded that WBC exposure had a positive effect on HRSD scores, and thus helped alleviate symptoms of depression. Given these results, the authors very recently published another study, similar to their previous work, which included a control group of 34 patients3. After 3 weeks, the HRSD scores for the 26 patients suffering from depression were reduced by 34.6% in the WBC group, against only 2.9% in the control group. One neurobiological hypothesis states that depression results from a deregulation of the hypothalamic-pituitary-adrenal axis (hypothalamo-hypophyso-adrenergic axis). The authors relate the improved mood regulation and HRSD scores to this axis. In addition, it seems that WBC also has positive effects on patients’ biological rhythms. All these results could provide some help for the temporary psychological problems frequently encountered by athletes during training.
CONCLUSIONS
The published studies concentrate on physiological, biochemical and haematological parameters affected by WBC. It reduces proinflammatory responses, decreases pro-oxidant molecular species and stabilises membranes, resulting in high potential beneficial effects on sports-induced haemolysis, and cell tissue damage, which is characteristic of heavy physical exercise. Conversely, it does not influence immulogical or hormonal responses, with the exception of testosterone, estradiol, noradrenaline and myocardial cell metabolism. Interleukin concentrations are modified by WBC, which induces anti-inflammatory responses.
In the context of recovery between two training sessions, it has showed that a single session of WBC performed shortly after a maximal exercise exerted a strong influence on parasympathetic reactivation, yielding a two- to four-fold augmentation of in pre-exercise vagal-related HRV indices, only 1 hour post-exercise. In addition to the desirable effects of WBC identified in sport, future research should aim to determine whether the strong influence of WBC on parasympathetic reactivation at the cardiac level could present additional benefits over longer periods, as fatigue accumulation during periods of intensified training has been associated with changes in the autonomic modulation of heart rate in athletes.
The published data are generally not controversial, but further studies are necessary to confirm the present observations. Standardisation of exposures times and the number of treatments during each cycle could improve data comparison. Due to the impact on the parasympathetic reactivation, we hypothesised that further studies conducted on sleep efficacy are needed in order to speed-up the recovery of elite athletes.
***************************************
Christophe Hausswirth, PhD is the Head of the Research Department and the Director of the Laboratory of Sport, Expertise and Performance, INSEP – French National Institute of Sport, expertise and Performance, Paris, France.
Contact: christophe.hausswirth@insep.fr
References
- Paddon-Jones DJ, Quigley BM. Effect of cryotherapy on muscle soreness and strength following eccentric exercise. Int J Sports Med 1997; 18:588-593.
- Hausswirth C, Louis J, Bieuzen F, Pournot H, Fournier J, Fillard JR et al. Effects of whole-body cryotherapy vs. far-infrared vs. passive modalities on recovery from exercise-induced muscle damage in highly-trained runners. PLoS One 2011; 6:e27749.
- Rymaszewska J, Ramsey D, Chladzińska-Kiejna S. Whole-body cryotherapy as adjunct treatment of depressive and anxiety disorders. Arch Immunol Ther Exp (Warsz) 2008; 56:63-68.
- Banfi G, Lombardi G, Colombini A, Melegati G. Whole-body cryotherapy in athletes. Sports Med 2010; 40:509-517.
- Schaal K, Le Meur Y, Bieuzen F, Petit O, Hellard P, Toussaint JF et al. Effect of recovery mode on post-exercise vagal reactivation in elite synchronized swimmers. Applied Physiology, Nutrition, and Metabolism 2013; 38:126-133.
- Swenson C, Swärd L, Karlsson J. Cryotherapy in sports medicine. Scand J Med Sci Sports 1996; 6:193-200.
- Lubkowska A, Chudecka M, Klimek A, Szyguła Z, Frączek B. Acute effect of a single whole-body cryostimulation or prooxidant-antioxidant balance in blood of healthy, young men. J Therm Biol 2008; 33:464-467.
- Pournot H, Bieuzen F, Louis J, Mounier R, Fillard JR, Barbiche E et al. Time-course of changes in inflammatory response after whole-body cryotherapy multi exposures following severe exercise. PLoS One 2011; 6: e22748.
- Vaile J, O’Hagan C, Stefanovic B, Walker M, Gill N, Askew CD. Effect of cold water immersion on repeated cycling performance and limb blood flow. Br J Sports Med 2011; 45:825-829.
- Stanley J, Buchheit M, Peake JM. The effect of post-exercise hydrotherapy on subsequent exercise performance and heart rate variability. Eur J Appl Physiol 2012; 112:951-961.
- Al Haddad H, Laursen PB, Ahmaidi S, Buchheit M. Influence of cold water face immersion on post-exercise parasympathetic reactivation. Eur J Appl Physiol 2010; 108:599-606.
- Westerlund T, Uusitalo A, Smolander J, Mikkelsson M. Heart rate variability in women exposed to very cold air (-110°C) during whole-body cryotherapy. J Therm Biol 2006; 31:342-346.
- Cholewka A, Drzazga Z, Kajewski B, Bogucki R, Wisniowska B. Thermal imaging of skin body surface die ti whole-body cryotherapy – preliminary report. Phys Med 2004; 1:81-83.
- Hausswirth C, Schaal K, Le Meur Y, Bieuzen F, Filliard JR, Volondat M et al. Parasympathetic activity and blood catecholamine responses following a single partial-body cryostimulation and a whole-body cryostimulation. PlosOne 2013; 8:e72658.
- Leppäluoto J, Westerlund T, Huttunen P, Oksa J, Smolander J, Dugué B et al. Effects of long-term whole-body cold exposures on plasma concentrations of ACTH, beta-endorphin, cortisol, catecholamines and cytokines in healthy females. Sca J Clin Lab Invest 2008; 68:145-153.
- Lubkowska A, Szyguła Z. Changes in blood pressure with compensatory heart rate decrease and in the level of aerobic capacity in response to repeated whole-body cryostimulation in normotensive, young and physically active men. Int J Occup Med Environ Health 2010; 23:367-375.
- Banfi G, Melegati G, Barassi A, Dogliotti G, Melzi d’Eril G, Dugué B, Massimiliano M et al. Effects of whole-body cryotherapy on serum mediators of inflammation and serum muscle enzymes in athletes. J Therm Biol 2009; 34:55-59.
- Rønsen O, Børsheim E, Bahr R, Klarlund Pedersen B, Haug E, Kjeldsen-Kragh J et al. Immuno-endocrine and metabolic responses to long distance ski racing in world-class male and female cross-country skiers. Scand J Med Sci Sports 2004; 14:39-48.
- Smolander J, Leppäluoto J, Westerlund T, Oksa J, Dugué B, Mikkelson M et al. Effects of repeated whole-body cold exposures on serum concentration of growth hormone, thyrotropin, prolactin and thyroid hormones in healthy women. Cryobiology 2009; 58:275-278.
- Nieman DC (1994) Exercise, infection, and immunity. Int J Sports Med 1994; 15:S131-S141.
- Dugué B, Leppänen E. Adaptation related to cytokines in man: effect of regular swimming in ice-cold water. Clin Physiol 2000; 20:114-121.
- Dugué B, Smolander J, Westerlund T, Oksa J, Nieminen R, Moilanen E et al. Acute and long-term effects of winter swimming and whole-body cryotherapy on plasma antioxidative capacity in healthy women. Scand J Clin Lab Invest 2005; 65:395-402.