Guest blog by sports physiotherapist @NicolvanDyk (Qatar)
“If there’s a fork in the road, take it.” Yogi Berra
Tiger Woods has officially withdrawn from the Ryder Cup – a move that makes a lot more sense than his starting the PGA last week. It seems like he is now following sound medical advice. A proper break aimed at full recovery. He is aiming to return in December for the World Challenge tournament, which seems reasonable. But what will happen beyond that. What does his future hold?
That was the question some colleagues asked me at the Aspetar Orthopaedic and Sports Medicine Hospital on Wednesday (prompted by a recent blog from Prof Karim Khan (@BJSM_BMJ). How would I advise perhaps the greatest golfer ever? Can we base it on evidence?
I am sure we can. Sports Medicine Physicians and Physiotherapists make such assessments every day, from elite level athletes to all the rest of us. Here’s a short proposal that may resonate with many Sports Medicine clinicians’ reasoning in this scenario. (And to Mr. Woods, I would hope to think your team is doing the same.) (And of course I’m keen to learn from those more expert than I).
- Correct Diagnosis (correction, hypothesis)
Let’s open the box and look inside. No, unfortunately no rabbit. It is rare for a single diagnosis to capture the full spectrum of what has transpired for an injury to happen. And no doubt, without any knowledge of the specific medical condition or advice Tiger Woods has received to this point, what we need to do first (or at least redo again) is work through some hypotheses, to make a proper clinical diagnosis.
Unfortunately another MRI scan would most likely not help us (see reference here). Imaging is useful, and there are a couple of things we want to exclude, but what we see must make sense in light of the whole clinical picture. As a suggestion, let’s call it a holistic assessment. We need to look at all the aspects influencing current pain experience, playing performance, and then do a full musculoskeletal examination looking at movement patterns and muscle recruitment, to understand the current condition. It needs to include history, both past and present, classification based cognitive functional therapy (CB-CFT), pain science education, nutrition and conditioning.
Our diagnosis will perhaps not be catchy, or sexy like “sacrum out” or “disc popped”, but it will be as accurate and inclusive as possible, (maybe something like “intervertebral joint dysfunction with movement restriction into flexion”) which will guide us in our treatment and rehabilitation. This sort of thinking allows different information to be taken into account, it creates the opportunity to evolve if needed (conditions change over time) and allow us to adapt whatever treatment we choose to utilize. This is necessary for achieving our goal. And yes, then do need to identify the goal, but hang on, we’ll get to that. We need to have something to test ourselves again, and some objective signs we can measure – other than eyeballing the sacrum.
- Correct Treatment and Rehabilitation
Unlike our colleagues in the 70s, 80s and 90s, we do not have to rely on expert opinion anymore. Not that expert opinion is not important, or valuable, but in the context of modern sports medicine, we have a growing body of evidence to support what we do, and why we do it.
And in this scenario, here is the key message – exercise works.
It is a proven therapy that has been found in most cases to trump the quick manipulation, magic tape or the odd bit of dry needling (or a hug). The scientific search here would lead you to mechanotherapy, or mechanotransduction, but let’s not be distracted by the details right now.
Research (see here a great editorial by Prof Peter O’Sullivan (@PeteOSullivanPT) on how we manage back pain) tells us to strengthen and rehabilitate the correct movement patterns (for the individual, no recipe’s needed, thanks) rather than spend hours rubbing lotion on your back, or cracking things into place. Firstly, perhaps most importantly, we need to ensure that you understand and comprehend the condition, the pain and what it means to you as a person. And then, perhaps as important, we need you to move, and move as well as you can. (Note to TW, the writer is a qualified manual therapist). Next, a gradual return-to-play programme where you build up the necessary strength, endurance and loading of the structures in your back so that when you get back, you really are “good to go.”
- Finding the TEAM that works towards injury free* peak performance
(*injury free = minimal risk of injury with maximum benefit from performance parameters)
Sports Medicine requires a team approach. And a good team will help you to integrate the evidence into a quality clinical decision. Of course I am not attempting to take away the complexities of these decisions in any way. But we have certainly come a long way from “the doctor said I shouldn’t play.”
Instead, we need to develop better algorithms to help make these decisions. Dr. Paul Dijkstra (@drpauldijkstra) has captured these difficulties in his open access BJSM article “Managing the health of the elite athlete: a new integrated performance health management and coaching model” highlights the difference when practicing integrated care medicine, and this article develops a health and performance grading system (see Table 3). This kind of system assists not only the Sports Medicine team, but it creates better understanding for the athlete of what all the information means.
Because related to rehabilitation that is (and should be) the main focus now, is performance. And having gone through 4 swing changes with 3 coaches in his career, Mr. Woods is hardly the same player as when he started. So has it backfired? And having the advantage of retrospection, was it worth it? Could these changes have influenced or played a part in the multiple knee injuries (and surgery) and ultimately the back injury leading to surgery this year?
Of course, the other question with any child prodigy who turns professional (and has a long, successful career) is load management. Prof Roald Bahr (@roaldbahr) from Norway suggests in a recent editorial for BJSM that “We now have the evidence to show that extra caution is needed when managing the gifted athlete.” Did we also fail Tiger Woods in this regard? Seeking to make the near perfect player even more perfect, asking too much of his gifted body?
Perhaps, although I am weary of the hindsight trap. We have to assess where we are now, and if we change anything again, it must be an integrated decision that allows ultimate performance with minimizing injury risk. Which brings us to perhaps the most pertinent question:
- The Risk-Reward Ratio – Will life after golf still allow playing some golf?
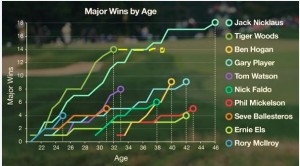
In 2008, aged 32, Tiger Woods had won 14 majors. It seemed likely (in an incredible fantastic way) that he would surpass Jack Nicklaus’ record of 18 majors. In December, when Tiger Wood plans to return, he turns 39. Is there still time? Jack Nicklaus was 46 when he won number 18, and a few other greats (Phil Mickelson, Ernie Els, Gary Player, Ben Hogan) have won majors in their 40s. But will he win another 5, with the rise of the young guns and the trail of injuries behind him? Mr. Woods wants to win majors, of that I am sure. But what will it take to win another four? What would be left? So here we have to ask, is the REWARD worth the RISK?
To really answer that question, we need to know from the athlete what the perceived reward is, versus the perceived risk. REWARD would be to hold the record number of major wins, to be the unchallenged greatest golfer that ever lived (if we classify greatest by number of major wins, although many might view Tiger Woods as the greatest already). REWARD would be to continue competing, and continue being the guy that everyone wants to beat (not sure if that’s true, but Jack Nicklaus still thinks so). REWARD could simply be to keep doing the thing you love to do, at the highest level. Yes, the rewards will be great. If this is indeed how TW sees the REWARD as well. So what then of the RISK?
There is a continuous effort among sports medicine researchers to identify risk factors for athletes, (e.g. IOC Injury Prevention Conference 2014). So when Sports Medicine Clinicians explain risk to an athlete, we try (or at least should attempt) to present all the information, and make the decision with all the components weighted. In this case, we have to consider the RISK of re-injury, of developing persistent pain, and dare I say, the RISK of not being able to continue playing golf at all? Have we even considered presenting out athlete with these scenarios? And more importantly, how we present this information, in a non-threatening and easy digestible way, might be crucial to the outcome
It’s a complex decision. But this needs thought, and all the possibilities considered. And I am not suggesting the answer is simple. Playing golf with the kids on a Saturday afternoon 20 years from now versus surpassing Jack’s record? (Oversimplification, I confess). It needs a sports medical team that is honest and clear, without seeking yes/no scenarios. (I would suggest this podcast by Prof Peter O’Sullivan here. He deals with the temptation to overdiagnose and overtreat brilliantly) And it would likely not be an “either/or” , but a “yes, and” answer that will allow the best outcome for the athlete.
As a sports physiotherapist, I wish Tiger Woods all the best with his rehabilitation and return to play. And I hope that he (and every elite professional athlete) will have the opportunity to make these decisions with the support of a good team and the value of current research and best practice guidelines driving the process.
Nicol van Dyk is a sports physiotherapist with special training in manual therapy. He is writing this in his personal capacity as a physiotherapist.
