By Drs James Thing & Thiviyani Maruthappu
Sport and Exercise Medicine: The UK trainee perspective (A twice-monthly Guest Blog)
As the sun finally breaks through the clouds after months of rain across the UK, it is worth reminding ourselves of the importance of sun protection for our athletes.
As a sports doctor I, like many others, regularly attend events over the summer months, weighed down by numerous medicines and medical kit. On occasion I am lucky enough to have packed my factor 30 sun protection lotion and try to apply at least once a day but what about those athletes roasting under our very noses?
Athletes who spend long hours in the outdoor sun, with little protection from long sleeved clothing are amongst the most susceptible of individuals
Excessive UV exposure occurs in sports such as: skiing, mountaineering, cycling, triathlon and other outdoor endurance events [1]. The knowledge of athletes regarding sun damage and protection tends to be good. However, their sun protection behaviours are often poor [2].
Excessive sun exposure is the strongest risk factor for many dermatological malignancies. This includes basal cell carcinoma, squamous cell carcinoma and malignant melanoma [3]
Malignant melanoma is on the increase. The diagnosis is being made three times more often now than in the 1980 s [4].
As well as excessive outdoor sun exposure, there is an increasing trend among young people to use tanning beds/booths. Athletes often feel under pressure to conform to aesthetic preconceptions. Many perform their events in minimal clothing and it is therefore important for them to feel confident in their appearance. A golden glow is often favoured to the pale complexion of an athlete who has suffered the effects of a long dark English winter (and summer!).
There are many daily use sunscreens on the market now that boast sport specific properties in their resistance to both water and sweat. As doctors responsible for the health of these athletes perhaps we should be pushing sun protection advice more aggressively?
Top 10 sun protection tips for athletes
1) Always use sun protection lotion when out between the 11am – 3pm
2) Ensure that sun protection lotion has both UVA (5*) and UVB cover (30+)
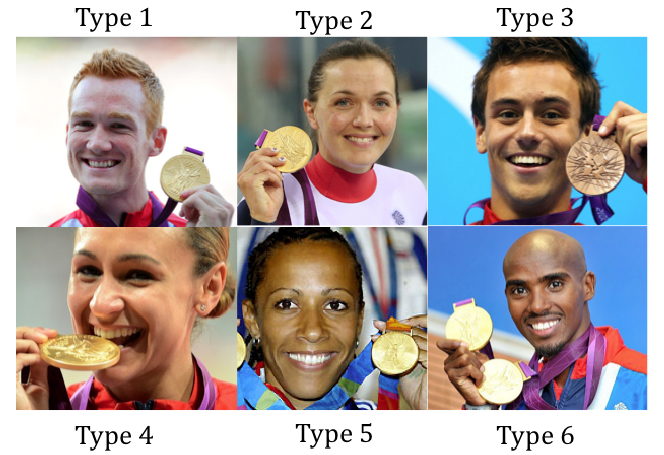
3) Know your skin type – type 1 skin is much more likely to burn than type 6, with “sunburn” increasing the risk of sun damage and subsequently skin cancer.
4) Know your burn time – the Sun Protection Factor (SPF) gives an indication of skin cover. Burn time (with sun protection lotion) = burn time (without sun lotion) x SPF
5) Consider using waterproof or ‘sport friendly’ sun lotion
6) Consider wearing a hat and long sleeved clothes (not always possible in sport)
7) Take extra care when exercising around water or snow as the reflection results in faster burn times.
8) Get to know your moles; monitor with regular digital photos if concerned.
9) Know your family history; malignant melanoma has a strong genetic component.
10) Avoid sunbeds, if concerned about appearance consider a good fake tan instead!
Resources
The “World UV” app was set up by the British Association of Dermatologists (BAD) and is free to download. It enables users to see the UV weather forecast and offers advice on how to avoid sun damage:
Useful patient information leaflets on skin type, self-monitoring of moles and sun protection advice are available here.
References
[1] Moehrle M. Outdoor sports and skin cancer. Clin Dermatol. 2008 Jan-Feb;26(1):12-5.
[2] Cohen PH, Tsai H, Puffer JC. Sun-protective behavior among high-school and collegiate athletes in Los Angeles, CA. Clin J Sport Med. 2006 May;16(3):253-60.
[3] Stenback F. Cellular injury and cell proliferation in skin carcinogenesis by UV light. Oncology 1975;32(2):61-75
[4] Accessed via http://www.cancerresearchuk.org/ on 22/08/2012
*****************************************************************
Dr James Thing is a Sport and Exercise Medicine Registrar in London. His clinical interests include rugby and athletics medicine.
Dr Thiviyani Maruthappu is a Dermatology Registrar in London and is a member of the British Association of Dermatology (BAD).