Guest blog by Prof @EvertVerhagen
It is well known that ankle sprains are the most common sports and physical activity (PA) related injury. It has also been clearly documented that athletes who experience an ankle sprain have a higher risk of re-injury within 1 to 2 years post-injury. This increased injury risk after an initial ankle sprain is generally thought to be caused by a proprioceptive impairment in the ankle due to trauma to mechanoreceptors of the ankle ligaments after an ankle sprain. Partly based on this rationale, neuromuscular training (NT) is widely used for rehabilitation after an ankle sprain, and is thought to improve proprioception by re-establishing and strengthening the protective reflexes of the ankle. However, despite a vast number of studies pointing towards the preventive effectiveness of NT, use of NT in practice does not seem to pick up. This leaves a high rate of ankle sprain recurrences that potentially can be prevented.
Consider the research cycle as postulated by Tugwell et al. [1] (Figure 1). In general this cycle states that effective prevention of injuries is the result from a sequence of seven translational steps, ranging in content form fundamental to practical. The first step is identifying the burden of disease and the seventh is evaluating a program that provides, by implementation, health benefits in the real world. If one substitutes ‘disease’ with ‘ankle sprains’, gaps arise in this translational research cycle. With regards to ankle sprains and NT there is an abundance of knowledge of step 1 (burden of disease) [e.g. 2-4] and a vast knowledge base on steps 4 (effectiveness) and 5 (cost-effectiveness) [5]. However, etiological (causation) and efficacy evidence is lagging behind, and implementation knowledge and program evaluation is completely lacking.
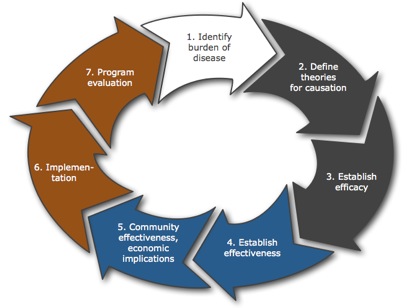
Figure 1 The research cycle of Tugwell et al.[17] In this model, there are seven distinct steps. The first is identifying the burden of disease and the seventh is evaluating the implementation of a program that provides health benefits in the real world (e.g. a prevention program for ankle sprains).
In my opinion, to push preventive in practice forward we require a more integrated and translational approach to bridge the gaps between on the one side effective preventive measures and the underlying working mechanisms, and on the other side between effective preventive measures and true injury prevention in every day practice (Figure 2). We need to take one step backwards in order to jump forward.
Recently we finished the 2BFit study, a RCT on the effectiveness of an 8 week unsupervised NT program for the prevention of recurrent ankle sprains [6,7]. This particular program was a further elaboration from a previous study we conducted [8,9]. In two studies this neuromuscular training program has now been proven (cost)effective for the prevention of ankle sprain recurrences. I dare to state that based on available evidence we now have an epidemiologically sound effective preventive NT program that can be used to unravel preventive pathways as well as effective prevention in practice.
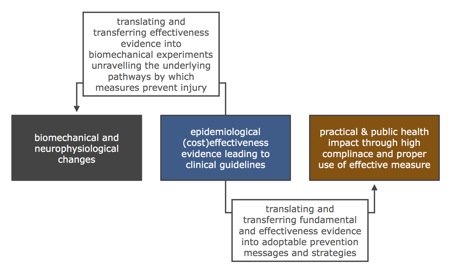
Figure 2 A schematic description of the proposed translational approach with a (cost) effective preventive measure as the starting point of fundamental and implementation goals.
Therefore, in a laboratory setting we can specifically study changes induced by the program in recently injured athletes, as compared to healthy athletes. This will provide information on which etiological factors are positively affected, which specific exercises of the program induce this effect, and the required frequency and duration of exercises for the NT program to be effective. The latter is required as the current effective NT program is a container of different exercises targeting strength, proprioception and agility in an 8 week program prescribing 3 exercise sets per week. Not surprisingly full compliance to prescribed program was low, even in controlled studies. Through this approach, fundamental knowledge will provide guidance to specify the NT program to it’s bare essentials and decrease user-burden while retaining full effectiveness. This will give us an effective and useable intervention message to be implemented.
References
- Tugwell P, Bennett KJ, Sackett DL et al. The measurement iterative loop: a framework for the critical appraisal of need, benefits and costs of health interventions. J Chronic Dis 1985;38:339–51.
- J Hootman, R Dick, J Agel Epidemiology of Collegiate Injuries for 15 Sports: Summary and Recommendations for Injury Prevention J Athl Tr 2007;42(2):311–319.
- Le Gall F, Carling C, Reilly T. Injuries in young elite female soccer players: an 8-season prospective study. Am J Sports Med 2008;36(2):276-84.
- William GF, Yard EE, Dawn C. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emer Med 2007;14(7): 641-5.
- Verhagen E, Bay K. Optimising ankle sprain prevention: a critical review and practical appraisal of the literature. Br J Sports Med. 2010;44(15):1082–1088.
- Hupperets M, Verhagen E, Van Mechelen W. Effect of unsupervised home based proprioceptive training on recurrences of ankle sprain: randomised controlled trial. BMJ 2009;339:b2684.
- Hupperets M, Verhagen E, Heymans M, et al. Potential savings of a program to prevent ankle sprain recurrence: economic evaluation of a randomized controlled trial. Am J Sports Med 2010;38(11):2194–2200.
- Verhagen EALM, Van Tulder M, Van der Beek AJ, et al. An Economical Evaluation of a Proprioceptive Balance Board Training Program for the Prevention of Ankle Sprains in Volleyball. Br J Sports Med 2005:39(2);111-115.
- EALM Verhagen, AJ van der Beek, JWR Twisk, LM Bouter, R Bahr, W van Mechelen. The Effect of a Proprioceptive Balance Board Training Program for the Prevention of Ankle Sprains. Am J Sports Med 2004:32;1385-1393.
*************************************************
Evert Verhagen is an Assistant Professor at the EMGO Institute for Health and Care Research at the VU University Medical Center, Amsterdam, the Netherlands. You can follow him on Twitter @EvertVerhagen