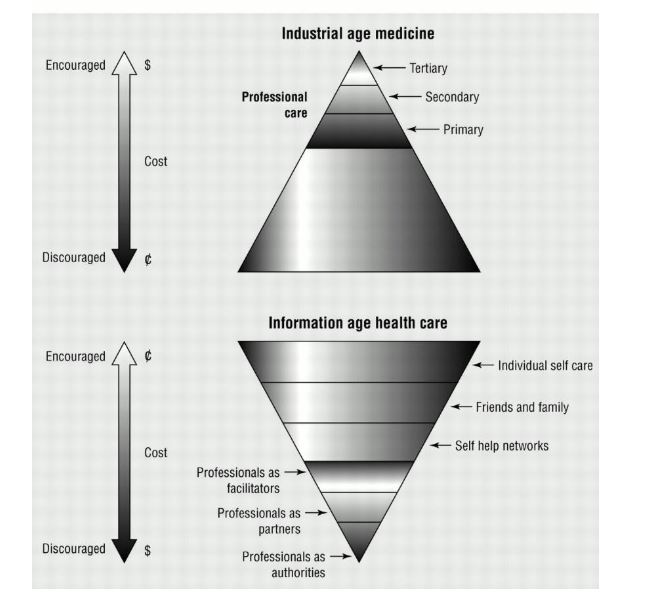
Almost a quarter of a century ago I wrote in The BMJ about an evolution from “industrial age medicine” to “information age healthcare.” Despite the spread of the internet, social media, and smartphones the evolution has gone very slowly, but now it’s happening in days.
The two types of health system are illustrated in the two triangles below: with industrial age medicine, professional care is dominant with hospitals at the top of the triangle consuming most resources; with “information age healthcare” the triangle is turned upside down, with much more emphasis on self-care and care from family, friends, and community—healthcare professionals are mostly facilitators and supporters, and sometimes—as with a patient in respiratory failure—acting as authorities.
The present pandemic of covid-19 cannot be managed in the traditional way with people taking their health problems to health professionals and being “managed.” People must stay away from the health system until they reach the point when they need aggressive hospital treatment. Most patients won’t reach that point, and it may be that the health care system will not have the capacity to treat even those who would benefit from hospital care. Families, carers, friends, and communities may have to cope without professional support.
The connection between the patients, their families, and the health system becomes hugely important, and people are using the phone, WhatsApp, Skype, email, instant messaging, whatever comes to hand.
I have a ringside seat with all this as I am the chair of Patients Know Best, a software company that brings together the records of patients from general practice, hospitals, mental health, and social care and puts them under the control of patients. The software allows direct communication between patients and the health system, and the communication ranges from online consultation through messaging to sharing of results and booking appointments. As its name implies, Patients Know Best is about genuinely shifting power and responsibility to patients, so ushering in “information age healthcare.”
We have contracts potentially to do all this for 10 million patients in the NHS, but for regulatory, bureaucratic, financial, anti-competitive, cultural, and technical reasons progress has been slow. The cultural blocks are probably the most important, and the technical ones the least important.
But the past few weeks have seen dramatic changes. For patients to benefit from Patients Know Best they have to be signed into the system. They must consent, and initially hospitals insisted that clinicians must gain the consent. Clinicians had other priorities, and things went very slowly. Next came kiosks and easier online ways for patients to sign up—and things have moved forward. But now the authorities are very keen to sign up patients and are gathering emails from wherever they can and emailing patients to register.
The software does allow online consultation using Skype, but this has not been much used. But “early adopter” clinicians have used messaging with patients. Health authorities have been nervous about this for various reasons—not least that there has been no payment to hospitals for online communication, meaning that more online and fewer face-to-face consultations means a drop in income. But now there is sudden enthusiasm for being able to communicate electronically with patients. The advantage of using Patients Know Best as opposed to a phone call or WhatsApp is that everything is recorded in the system alongside the patient’s records and can be seen by all those caring for the patient.
One of the main ways that Patients Know Best has been used is for sharing results of tests and investigations with patients. This can happen in real time as soon as patients are registered with the system, but there has been great reluctance to do so immediately, although some have done so. Health authorities have thought that patients must be told about test results face to face. All our experience, however, is that patients want results as quickly as possible, even when the news is bad. The results are accompanied by an explanation of what they mean.
Again the reluctance has disappeared, and many health authorities are seeking to share results as quickly as possible. Everybody can see the benefit of sharing the result of a test for covid-19 as quickly as possible whether it is negative (most at the moment) or positive.
The software is also used for care planning, but again progress has been slow. The care is often planned by the health professionals, and patients have had nothing to take home. Now there is great enthusiasm from care planning, encouraging patients to play a bigger role in their care of all their conditions and certainly with infection with covid-19. Patients Know Best used NHS guidance to prepare a template to help patients know what to do in the different stages of covid-19 infection.
Patients Know Best can also be used for advance care planning. This is particularly important when anybody could very soon find themselves close to death with difficult decisions to be made by their families and carers. So far there has been little use of this facility, but the time has surely come when as many people as possible should have an advanced care plan—and one that can be accessed by whoever might be caring for a patient who may die. (Many wealthy people have moved to their homes in the country to reduce their chances of being affected.)
A final possibility that may be particularly important in the pandemic is monitoring of patients’ vital signs at home. Current Health is a company that supplies the equipment for monitoring, and the results are communicated through Patients Know Best. So far it has been used when discharging patients, but it could be used to monitor patients at home with covid-19 who may be at risk of rapid deterioration.
We are still in Britain at the beginning of the pandemic, but already the NHS is beginning to move rapidly towards “information age healthcare.” And there will be no going back.
Richard Smith was the editor of The BMJ until 2004.
Competing interest: RS is the unpaid chair of Patients Know Best, but he has equity in the company.