 Reading about the idea of a minimal clinically important difference (MCID), I came across another term, less widely used: the patient acceptable symptom state or PASS.
Reading about the idea of a minimal clinically important difference (MCID), I came across another term, less widely used: the patient acceptable symptom state or PASS.
The earliest reference to this term that I have found, in PubMed and other databases, is from 2005, although the underlying concept antedates this. For example, at the OMERACT conference in 2003, dealing with outcome measures in rheumatology, there was discussion of whether improvement in pain is more important than improvement in function or vice versa, and how patients balance improved outcomes from a treatment against its adverse effects when deciding whether a therapeutic intervention is acceptable. Unsurprisingly, patients with joint diseases want both relief of pain and improved function.
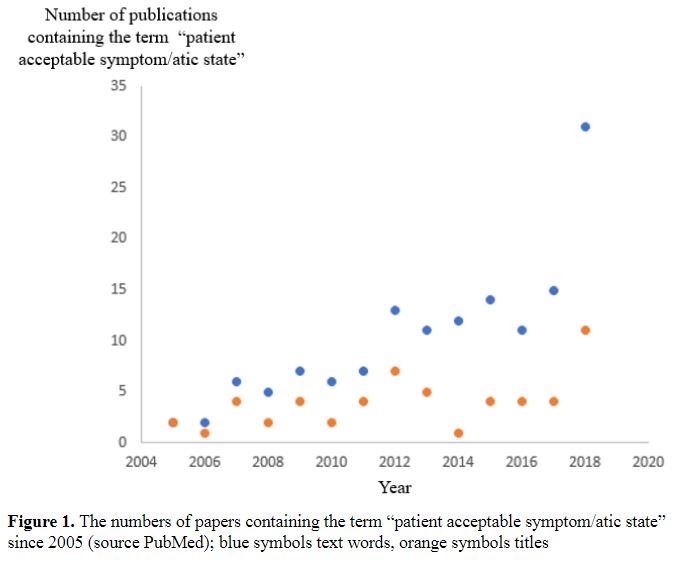
As Figure 1 shows, the term “patient acceptable symptom state” has not been widely used, with a current total of only 137 hits in PubMed at a median of nine per year, although there has recently been a small upturn, with 31 hits in 2018 and already 27 in 2019. Most of the publications deal with either rheumatology or joint surgery.
The “patient acceptable symptom state” has been defined as “the value beyond which patients consider themselves well” and, more precisely, “the highest level of symptom beyond which patients consider themselves well”. However, there is a difference between being well and being better. The former implies complete recovery while the latter admits the possibility of residual disability. And what is merely acceptable need not be what is desirable.
The difference between the minimal clinically important difference and the patient acceptable symptom state has been said to be that the former deals with whether and to what extent the condition is improved, while the latter deals with whether the change is acceptable to the patient. However, the definition of the minimal clinically important difference is “the smallest difference in score in the domain of interest which patients perceive as beneficial and which would mandate, in the absence of troublesome side effects and excessive cost, a change in the patient’s management”. It is hard to see how that differs substantially from the patient acceptable symptom state, assuming that what patients perceive as beneficial is also what they consider to be acceptable, even if only minimally. It seems unlikely that anyone who perceives a benefit would not consider it acceptable or that anyone with a change that they consider to be minimally acceptable would not also consider it to be beneficial. In fact, the assertion that the minimal clinically important improvement is the change required to achieve the patient acceptable symptom state unites the two terms.
Two disadvantages of the term “patient acceptable symptom state” are the difference between “acceptable” and “desirable” and that it is restricted to symptoms, ignoring signs. A patient with scalp psoriasis or a facial haemangioma, for example, might consider the lesions cosmetically undesirable, even if they caused no symptoms by themselves. Sacrificing the acronym, we might change “acceptable symptom” to “desirable outcome”.
Two disadvantages of the term “minimal clinically important difference” are that it does not focus sufficiently on the patient, which, as I have previously discussed, can be at least partly mitigated by omitting the word “clinically”, and that it does not distinguish between beneficial and harmful differences, despite the inclusion of the word “beneficial” in the definition. Awareness of this has led some to use the term “minimal clinically important improvement”. However, it might be better to separate the two concepts more explicitly, and to refer to minimal benefit and maximal harm.
This in turn suggests two new terms, which encapsulate all of these ideas and eliminate the disadvantages of the current terms: the minimal desirable benefit of a treatment and the maximal acceptable harm, where the latter is a composite of the harm of intervening and the harm of not doing so.
Then the benefit to harm balance of an intervention could be regarded as the extent to which the former outweighs the latter (a favourable balance) or the latter outweighs the former (an unfavourable balance).
Jeffrey Aronson is a clinical pharmacologist, working in the Centre for Evidence Based Medicine in Oxford’s Nuffield Department of Primary Care Health Sciences. He is also president emeritus of the British Pharmacological Society.
Competing interests: None declared.
