 Which is better: “Aspirin can cause Reye’s syndrome” or “Aspirin may cause Reye’s syndrome”? The answer lies in a consideration of modal verbs, also called modal auxiliaries.
Which is better: “Aspirin can cause Reye’s syndrome” or “Aspirin may cause Reye’s syndrome”? The answer lies in a consideration of modal verbs, also called modal auxiliaries.
Modal verbs are used to express modality, in other words, they modify the meaning of a verb, indicating how to interpret it. The main (or central) modal verbs are “can”, “could”, “shall”, “should”, “will”, “would”, “may”, “might”, and “must”; the semi-modal (or marginal modal) verbs are “ought to”, “used to”, “dare [to]”, and “need [to]”. They have three uses.
- Epistemic modal verbs (Greek ἐπιστήμη, knowledge) express the truth or likelihood of a proposition, i.e. whether it is possible, probable, or necessarily true. For example: “Aspirin may cause Reye’s syndrome” [in general, with a particular probability]; “Aspirin might cause Reye’s syndrome” [in this case, with a particular probability]; “The aspirin must have caused Reye’s syndrome” [for certain, in this case].
- Deontic modal verbs (Greek δέον, binding) express directives or permission. For example: “You must prescribe aspirin” [an imperative]; “You should or ought to prescribe aspirin” [preferably, unless something dictates otherwise]; “You may prescribe aspirin” [in this case, if it seems appropriate]; “You might prescribe aspirin” [in general, if it were indicated]; “I don’t dare prescribe aspirin for this child”; “You need not prescribe aspirin in this case”.
- Dynamic modal verbs (Greek δύναμις power or strength) ascribe ability or volition. For example: “Aspirin can cause Reye’s syndrome”.
There is much ambiguity in these words. For example, although “can” strictly speaking denotes ability, knowing how to or being able to, it is also used to denote possibility (“Yes we can”, which implies both ability and possibility) or permission (“Yes, you can”).
If you say “Aspirin can cause Reye’s syndrome”, you are implying that there is a known cause and effect association between the drug and the event, in other words that aspirin is capable of causing the syndrome, as is generally accepted.
On the other hand, if you say “Aspirin may cause Reye’s syndrome” in a general sort of way, you are implying that the association is suspected but not proven. If you say it in relation to an individual, you are implying that the use of aspirin in this case is a hazard, with a chance of harm. In both cases you will have some sort of probability in mind.
There is little doubt about all this in the case of aspirin, but if you were to say that a new medication “can” cause some adverse reaction, you might be accused of falsely implicating the medicine as a general cause of the reaction, if the evidence was not satisfactory or contended. It would generally be better in that case to say “may” or “might”.
As I have previously pointed out, the UK’s General Medical Council defines the words “must” and “should” in relation to its various pieces of guidance for doctors, as follows:
- “‘You must’ is used for an overriding duty or principle.”
- “‘You should’ [prefaces] an explanation of how you will meet the overriding duty.”
- “‘You should’ is also used where the duty or principle will not [always] apply, or where . . . factors outside your control . . . affect whether or how you can follow the guidance.”
Now, in its Prescribing guidance: Reporting adverse drug/device and other patient safety incidents, the GMC writes “You must inform the MHRA [the medicines regulatory agency in the UK] about . . . serious suspected adverse reactions to all medicines and all [sc. suspected] reactions to products marked with a Black Triangle in the BNF and elsewhere using the Yellow Card Scheme.” However, reporting in this way is not mandatory in the UK. It is mandatory in some countries, such as France, Denmark, and Korea, but in Japan the proposed introduction of a mandatory system for reporting fatal adverse events led to widespread fear of prosecution and defensive medicine; physicians started to refuse to see high risk patients and referrals to other hospitals became widespread; medical school graduates began to avoid specialties that were perceived as being legally particularly vulnerable, and various hospitals and clinics had to close.
It’s not that UK doctors must not report suspected adverse reactions, but not that they must.

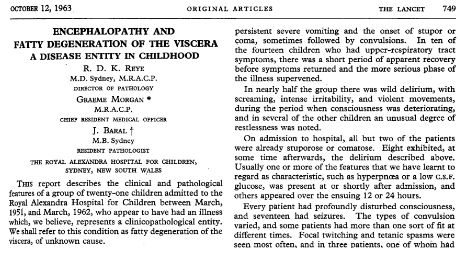
Ralph Douglas Kenneth Reye (1912–77), who, with Graeme Morgan and Jim Baral, described what we now call Reye’s syndrome in 1963 (Reye RD, Morgan G, Baral J. Encephalopathy and fatty degeneration of the viscera. a disease entity in childhood. Lancet 1963; 2(7311): 749-52); I guess that the surname Reye (pronounced rye) is a variant of the Spanish word for a king, rey.
Jeffrey Aronson is a clinical pharmacologist, working in the Centre for Evidence Based Medicine in Oxford’s Nuffield Department of Primary Care Health Sciences. He is also president emeritus of the British Pharmacological Society.
Competing interests: None declared.
