Recent headlines have indicated NICE’s displeasure at how it has been asked to implement value based pricing. The stories are based on a paper, “Value based assessment of health technologies,” which was considered by the NICE board on 22 January.
The paper proposed two main changes:
a) an alternative approach to the Wider Social Benefit proposed by the Department of Health, based on “the shortfall in the ability of people to contribute to society as a result of their disease or condition.”
b) incorporation of burden of illness based also on the “shortfall.”
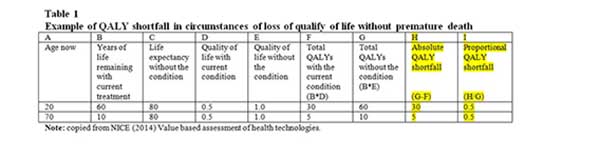
Both changes rely on the concept of a “quality adjusted life year (QALY) shortfall,” which can be estimated in two ways: an absolute and a proportional shortfall. These are best illustrated in table 1 of NICE’s paper. The absolute QALY shortfall for a 20 year old in Table 1 is the QALY loss due to the condition with current treatment compared with maximum QALYs without the condition (column H). The proportional QALY loss for the same individual is 0.5, based on the absolute loss divided by the maximum QALYs without the condition (column I). The absolute QALY shortfall is related to age, unlike the proportional shortfall, as shown, considering how these figures work for a 70 year old. Such a person faced with the same condition would have an absolute QALY shortfall of 5 but, a proportional QALY shortfall of 0.5.
“Wider social benefit” is rejected on the basis that it inevitably takes age into account to some extent.
NICE proposes using the absolute QALY shortfall calculated instead of wider social benefit. “This societal shortfall defines the loss in an individual’s societal function as a result of living with a disease or condition compared with the total amount of future societal function possible without the illness. The higher the shortfall, the larger the impact of future societal function.”
This differs from the Department of Health approach. By focusing on the health loss due to a condition, and not on the effects of the condition on production and consumption, it measures the notional loss, in QALYs, to a person from having a disease/condition, with existing treatment regardless of any new treatment. It can be seen as a loss of life expectancy (quality adjusted). Absolute QALY shortfall will overlap with the economic gains/losses due to having a disease/condition and is presented in the paper as a proxy for these.
Proportional QALY shortfall is proposed as the basis for adjusting QALYs for burden of illness (severity) by reference to the adjustments NICE currently makes for end of life drugs. It is defined as the absolute QALY shortfall, as above, divided by the total QALYs without the condition. This makes it largely insensitive to the age at which people are diagnosed. The proportional QALY shortfall rises as people approach the end of life, enabling it to be linked to higher weights for end of life treatments.
The paper makes the case for adjusting QALYs for burden of illness on a survey of 3000, which supported “the notion that when a choice needs to be made, providing treatment to people with a larger burden of illness is a higher priority than for those with a lower burden of illness.” However, lacking a sufficient empirical basis for these, the paper proposes that the NICE advisory committee be given discretion on its implementation. The paper does not note the failure of several surveys to find public support for giving higher priority to those near the end of life.
Instead of establishing a higher cost per QALY threshold for assessing new health technologies, this approach would vary the value of a QALYs by condition, using both absolute and proportional shortfall. As always, winners and losers will emerge, but the paper does not identify these.
Comments and thoughts
Firstly, this is ingenious in seeing off the wider social benefits as defined by the Department of Health. Using absolute QALY shortfall as a proxy for wider social benefits has the major advantage of retaining the currency of QALYs and without the equity objections of wider social benefits. QALY shortfalls would be estimated along the lines of what the Department of Health proposed for all conditions/diseases. It would imply a higher weighting for conditions that imposed the greatest QALY loss. For example this would attach an extra value to being severely handicapped, a condition which under wider social benefits could have suffered a reduced value owing to not being employed.
Secondly, proportional QALY shortfall can be related to NICE’s end of life criteria for the simple reason that the ratio rises towards the end of life. How this proportional shortfall approach will incorporate the burden of illness remains to be established.
Thirdly, the proposed alternative approach to wider social benefits solves the problems of some treatments leading to higher costs due to maintaining patients in poor value health states. This has been a concern to pharmaceutical companies. Industry seem likely to support the proposed changes.
Fourthly, the entire process of establishing relative cost effectiveness of interventions is going to become less transparent. Not only will the incremental cost per QALY have to be established, but so too will the absolute and proportional QALY shortfall of the condition. The phrase “A QALY is a QALY is a QALY” will have to be replaced by “The value of a QALY depends on the absolute and proportional QALY shortfall of the condition.” Data will be required on QALY shortfalls for the entire spectrum of diseases and conditions. This may be helped by the improved Disability Adjusted Life Year (DALY) value for 291 diseases and injuries published in 2013. Indeed, the focus on shortfall will have the effect of making QALYs more like DALYs.
Fifthly, NICE’s proposed way forward is only partly evidence based. The benefits in cost benefit analysis need to be supported by evidence that they reflect the value of the public. No such support has been shown for the end of life criteria despite several contradictory surveys, yet they will be incorporated into the new QALYs. While surveys have shown some support for including burden of illness, the extent to which that is captured by proportional QALY shortfall remains to be shown.
Sixthly, the proposed way forward keeps the cost per QALY approach alive, but with amendments that even supporters will struggle to explain. All the adjustments will be on QALYs, leaving costs unchanged. That variant of cost benefit analysis, which uses cost per QALY (instead of some measure of willingness to pay) lives on. Dubbed “extra welfarism,” it has proved less bad than its alternatives.
Seventhly, the publicity around these proposed changes has focused on the implications of wider social benefits discriminating against the elderly people. Absolute QALY shortfall will also discriminate against age, but offset to some unknown extent by proportional QALY shortfall. It is hard not to laugh at Conservative MPs describing this element of Andrew Lansley’s value based pricing as “barking mad.”
Finally, this proposed policy, by continuing to give higher QALY values to patients approaching their end of life, despite any evidence that this is supported by the public, means that it will impose substantial and unwarranted ongoing costs to the NHS.
James Raftery is a health economist with several decades experience of the NHS. He is professor of Health Technology Assessment at Southampton University. A keen “NICE-watcher,” he has provided economic input to technical assessment reports for NICE but has never been a member of any of its committees. The opinions expressed here are his personal views.