Tennis elbow (or lateral epicondylitis) is a common upper limb condition seen in the musculoskeletal (MSK) clinic. It can cause significant pain, restriction to activity and impact patients Quality of life (QoL). Despite the name, it has little to do with tennis and our understanding of this condition has led us to appreciate the wider metabolic, degenerative, overuse and inflammatory risk factors involved.
Rather than being a single condition with a defined set of risk factors to optimise – MSK clinicians should adapt a personalised and targeted approach to treatment. This should consider the loading potential, metabolic health and Otho biologic, injection and orthopaedic interventions.
Going beyond overuse and inflammation theories
Tennis elbow was traditionally thought of as an overuse injury, that occurs in patients where the common extensor tendon is being challenged beyond its mechanical capacity (1). Varying degrees of inflammation or degeneration have also been proposed as contributing factors to the condition and they can influence decisions about treatment options.
Breaking down tennis elbow: what do we know about common risk factors?
Newer theories of tendon related pain (tendinopathy) have helped us move away from pure imaging or histology-based criteria. Chronic sensitisation (1), neurogenic sensitisation, menstrual (2) and metabolic health (2) have all been linked to tendon related pain and are important risk factors to be aware of alongside known intrinsic and extrinsic risk factors:
| Tennis elbow risk factors | |
| Intrinsic risk factors | Extrinsic risk factors |
| No gender bias (3) | Work/daily function requirements (4) |
| Metabolic syndrome (5) (hypertension, dyslipidaemia (6), type II diabetes) (7) | Sport technique (8) |
| Age 30-50 (9) | Racquet factors (10,11) e.g. quality, string tension |
| Increased carrying angle (12) | Sporting load management |
| Muscular imbalance between rotator cuff/scapula and wrist flexors and extensors13 | Smoking (5) |
| Alcohol (5) | |
| Menopause, perimenopause (14,15) | |
Table 1: Tennis elbow risk factors

Figure 1: A summary poster of intrinsic and extrinsic risk factors for tennis elbow
Tennis elbow: How common is it ?
- Tennis elbow – annual incidence of 30 to 45/10,00016
- It is estimated that only ½ of patient’s with symptoms seek medical review16
- 89% of patients improve within 1 year17
- Tennis elbow is predominantly a self-limiting condition with ½ of patient’s improving every 3 months17
- It is rarely seen in adolescents or older adults >65
In the initial stages of tennis elbow, the consensus is that:
- a clear diagnosis should be made and
- early rehab treatment offered.
Most guidelines support physiotherapy for 3 months +/- short courses of NSAIDs with stomach protection (PPI medications). Providing patients with appropriate timeline for healing, can help to set the horizon for how long to treat the condition conservatively for. It can also aid shared decision-making discussions regarding the risks and benefits of interventions, for resistant cases that are impacting QoL/function.
Subtype the risk factors: to help guide treatment decisions!
For resistant cases, presenting to MSK services, we propose a clinical decision tool to help subtype risk factors, and who may need further imaging or metabolic work up.

Figure 2: A summary poster of the risk factors and management of tennis elbow
FCP / APP – Assessment toolkit
During the initial assessment it is important to confirm the diagnosis and rule out significant red flag symptoms. In the UK first contact practitioners (FCP), typically undertake this assessment in primary care either virtually or face to face.
| Red Flag symptoms | |
| History of Trauma, swelling or dislocation | Fractures, dislocations (Pulled Elbow) |
| Swollen, Red & tender Joints, systemic symptoms, recent infection. | Septic arthritis |
| Rapid increasing Mass/ Swelling. | Malignancy |
| Bilateral, swelling, stiffness, redness and warmth | Inflammatory arthritis |
| History of trauma or surgery, swelling. Lump & loss of range of motion | Heterotopic ossification. |
Table 2: Red flag symptoms associated with tennis elbow
Although rare, tennis elbow has a mean duration of 6-48 months (18) meaning that patients are committed to treatment for an extended period. Focussed clinic-based test and history can help to rule out common differentials that may be a mimicking cause or co-exist with tennis elbow. It is important to identify these early as it may help to tailor management as part of a shared decision-making process.
| Nerve Related Elbow Conditions & other Differential Diagnoses | |
| Cervical referred pain or radiculopathy | -Radiating pain from cervical spine, reproduced with active and/ or passive neck movements.
-Positive Spurling’s sign. -Focal Myotome, dermatome and/ or reflex deficits present of affected nerve. |
| Radial Tunnel Syndrome | -Pain with resisted wrist extension and supination.
-Pain 3-4 cm distal and anterior to lateral epicondyle. -Diffuse pain, rarely sensory or motor changes |
| PIN Compression Syndrome | – More common in manual labourers, males and bodybuilders
– Clinically presents with weakness of thumb and wrist extensors without sensory deficits. -Presents with pain in distal forearm and wrist and sometimes proximally. |
| Elbow Arthritis | -Joint pain with or with loss of range of motion.
-History of trauma or of heavy manual or sporting use. |
| Posterolateral rotatory instability | -Caused by persistent insufficiency of the lateral collateral ligament (LCL) complex, most notably the lateral ulnar collateral ligament (LUCL).
-History of trauma, rarely overuse -Pain, clicking, snapping, and/ or feeling of instability during elbow flexion/extension with forearm supinated. -+ve Posterolateral rotatory instability Test. (Posterolateral Rotatory Instability Test (Whitworth Athletic Training) – YouTube) |
Table 3: Nerve-related elbow conditions & other differential diagnoses
Clinic based assessment – for tennis elbow
| Key clinical history questions | Key clinical tests (with sensitivity and specificity) | Key imaging changes – on US and MRI |
|
-Pain on palpation of lateral epicondyle
-Maudsley’s (Maudsley’s Lateral Epicondylitis Test⎟Lateral Epicondylitis or Tennis Elbow (youtube.com)). Sensitivity: 88%, specificity 0% (19) -Mills (Mill’s Test | Lateral Epicondylitis or Tennis Elbow (youtube.com)). Sensitivity: 53%, specificity: 100 % (19) -Cozen test (Cozen’s Test | Lateral Epicondylitis | Tennis Elbow Diagnosis (youtube.com)) Sensitivity: 84%, specificity: 0% (19) -Muscle weakness is found in tennis elbow. Pain free gripping was reduced by about 60% compared to non-affected side (20) -If the patient reports clicking or locking, consider imaging used to detect other pathologies, such as loose bodies, articular cartilage damage, ligament injury, or elbow synovial fold (plica) syndrome |
Ultrasound:
Affected tendon may demonstrate focal areas of hypo-echogenicity, show tears, intra tendon calcification or thickening and doppler flow suggestive of hyperaemia. Bony irregularities at the tendon insertion may also be seen. Epidemiological studies demonstrate that up to 54% of asymptomatic populations have ultrasonographic features suggestive of tennis elbow. It is a sensitive but not specific modality and thus can be useful to rule out, rather than rule in tennis elbow (21). |
Table 4: Clinic based assessment – for tennis elbow
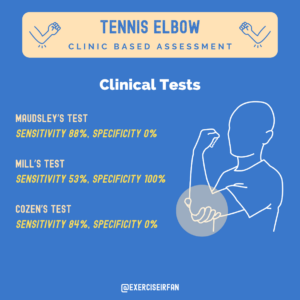
Figure 3: A summary poster of key clinical tests for tennis elbow

Figure 4: Maudsley’s test being performed

Figure 5: Mill’s test being performed, whereby examiner stabilises patient’s forearm with one hand and the same hand’s thumb to palpate the lateral epicondyle, whilst the examiner’s other hand passively pronates the forearm

Figure 6: Continuation of Mill’s test where examiner then flexes the patient’s wrist and extends the elbow maximally, which places tension on extensor carpi radialis brevis to exacerbate symptoms
The role of imaging
Where available and as part of a clinical work up, ultrasound can provide additional details of the tendons affected. Tendon tears, tendon thickening, calcification and neo-vascularisation are all features that can be assessed for on ultrasound and compared to the contralateral side.
Diagnostic accuracy of the characteristic ultrasound findings for Lateral Epicondylar Tendinopathy (LET)
| Characteristic ultrasound findings | Sensitivity (%) | Specificity (%) | |
| Common Extensor Tendon Thickening (21–24) | – | – | |
| ≥ 4.2 mm | 78.4 | 95.2 | |
| ≥ 4.85 mm | 90.5 | 85.7 | |
| +10% difference between symptomatic and asymptomatic side | 70 – 72 | 52 – 67 | |
| Common Extensor Tendon Tear (25,26) | 14 – 64.5 | 85.2 – 100 | |
| Neovascularisation (21,24,26–28) | – | – | |
| Via Power Doppler | 19 – 81 | 77 – 100 | |
| Via Colour Doppler | 57 – 95 | 88 – 100 | |
| Calcification (21,26) | – | – | |
| Internal | 7 – 33 | 83 – 100 | |
| External | 45 | 90 | |
| Hypoechoic changes (21,24,26,28,29) | 53 – 92 | 60 – 100 | |
| Cortical Irregularities (23,24,26,28) | 18 – 63 | 63 – 100 | |
| Elasticity (22,29–31) | – | – | |
| Shear-wave elastography (SWE) | 90.5 – 100 | 89 – 93 | |
| Compression sonoelastography (SEL) | 78 | 92 | |
| Ultrasonography (US) | 95 | 89 | |
Table 5: Diagnostic accuracy of the characteristic ultrasound findings for Lateral Epicondylar Tendinopathy (LET)
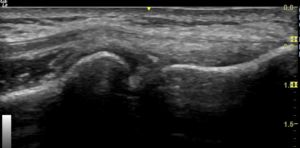
Figure 7: Normal US scan of the common extensor origin – lateral elbow
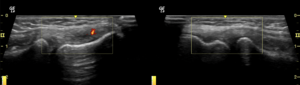
Figure 8: Dynamic US allows for the comparison of symptomatic side (left) versus unaffected side (right)

Figure 9: Ultrasound examination of the lateral elbow in Mill’s testing

Figure 10: Ultrasound examination of the lateral elbow in resisted finger extension positions
Treatment options (3)
- Primary care: assessment and establishing any red flags – imaging is not required unless considering alternative diagnosis.
- Primary care: patient education, exercise sheet, activity modification, topical anti-inflammatories for a month, avoid corticosteroid injections. Reassurance that this is self-limiting and symptoms should resolve in three months. If no improvements in 6-12 weeks, refer to local physiotherapy.
- Physiotherapy: assessment (check red flags again), stretching exercises, eccentric loading extensor tendons. If no improvement within 12-24 weeks, MSK / Orthopaedic referral for further assessments. Imaging with US/ MRI – can help to assess for inflammatory features, significant tears or changes to the underlying joint if suspected.
- Secondary care: due to self-limiting nature, we anticipate the prior 3 steps would help 50% of patients to recover within 3 months. Further treatments can be offered but studies offer mixed evidence of benefit for orthotics, PRP injections, dry needling and surgery. Surgery options include open or arthroscopic techniques.

Figure 11: MSK playbook summary diagram for tennis elbow pathway
Steroid injections
Injection therapies can play an important role in the management of elbow tendinopathy when other conservative management strategies have failed to achieve adequate symptom control. Historically, corticosteroid injections have been used to help decrease pain and symptoms. While steroid injections are effective in the short term, there is less evidence for their long-term benefit. Repeated injections may also negatively impact soft tissue structures and tendon integrity. Providers should carefully monitor the total steroid burden and be mindful of the frequency of injections to avoid harm.
Novel therapies
There is a growing body of evidence supporting the use of platelet rich plasma (PRP) injections for the treatment of elbow tendinopathy. A recent meta-analysis (32) concludes that while corticosteroid injections provide better short term relief (<2 months), PRP injections provide far better long term (>6 months) functional improvement and pain relief. Other meta-analyses33 have similar conclusions, that PRP has “no advantage over steroid injections within the first month of treatment, but that it is superior to steroids at both 3 and 6 months.”
One systematic review (34) compared PRP injections to lateral epicondylar surgery and found that in comparison to surgery, “PRP injections offer similar improvements in pain and function for patients suffering from lateral epicondylitis, especially in the short- and mid-term.”
Extracorporeal shockwave therapy (ESWT) is another option gaining attention for the treatment of elbow tendinopathy. A recent meta-analysis (35) examining the effectiveness of shockwave therapy on various tendinopathies reports that shockwave can be a highly effective therapy option for relieving pain in people with tendinopathy, including lateral epicondylitis. However, more clinical trials are needed to determine optimal treatment sessions, pulse intensity, and frequency.
Surgical options for tennis elbow
Current evidence (3) shows there is no evidence of benefit of surgery compared to placebo, and as such, surgery for tennis elbow is uncommon. In rare acute cases where there is a sudden traumatic incident (tear) and an underlying healthy tendon, then acute surgical management may be considered.
The two main surgical approaches are open and arthroscopic, and the most popular option in each is extensor release +/- debridement. Of the two approaches, current evidence (36) suggests there is no difference in outcome (visual analog pain score, patient-rated tennis elbow evaluation score, grip strength) when either arthroscopic and open surgical approaches were used. If surgery is performed, early post-operative rehabilitation is key to prevent stiffness with activity modification as appropriate (37).
Conclusion
- Tennis elbow is a self-limiting condition, that has favourable outcomes with time and appropriate rehab that addressed triggering risk factors in the patient’s daily activities, work, and hobbies
- In resistant cases >3 months, consider subtyping the tennis elbow into one or more categories- (degenerative, overuse, metabolic and inflammatory). This can help personalise discussion about treatment options
- Current evidence for tennis elbow shows mixed evidence, and shared decision-making discussions should include discussion on risks, benefits, healing potential, and avoidance of harm.
- OrthoBiologics (PRP) injections are a new injection options, that avoids steroid burden and can improve pain scores over the medium and long term.

Figure 12: Tennis elbow pathway summary diagram
Names of authors
Miss Geethana Yogarajah
6th Year Medical Student
University of Cambridge
LinkedIn: https://www.linkedin.com/in/geethana-y-9b134327b
Mr Muhammad Umer
5th Year Medical Student
King’s College London
LinkedIn: www.linkedin.com/in/muhammad-umer19/
Mr Ryan Linn
Final Year Medical Student
University College London (UCL)
Twitter: @Ryan_Linn_
Mr Niel Kang
Consultant Trauma & Orthopaedic Surgeon
Cambridge University Hospitals NHS Trust
Affiliate Assistant Professor
Clinical School of Medicine, University of Cambridge
Education and Careers Committee
British Orthopaedic Association
Twitter @kangstagram77
Mr Mark Moriarty
Health advisor
BUPA St Albans
Ms Ciara Murphy
Health advisor
BUPA St Albans
Mr Joe Askew
Advanced Physiotherapist Practitioner Lead Bupa Health Clinics
Dr Anoop Raghavan
York City FC
Mr Hozefa Dahodwala
Advance Practice Physiotherapist
MSK Sonographer & Non-Medical Prescriber
Dr Jeffrey Peng MD, CAQSM
Sports Medicine Physician
Clinical Assistant Professor (Affiliated); Stanford University School of Medicine, Department of Medicine, Division of Primary Care & Population Health
Twitter: @JeffreyPengMD
YouTube: youtube.com/c/JeffreyPengMD
Mr Joe Askey
Advanced Physiotherapist
Practitioner Lead Bupa Health Clinics
Dr Irfan Ahmed
Consultant in Musculoskeletal, Sport & Exercise Medicine,
Twitter @ExerciseIrfan
Bibliography
- Fernández-Carnero, J., Fernández-de-las-Peñas, C., de la Llave-Rincón, A. I., Ge, H.-Y. & Arendt-Nielsen, L. Widespread Mechanical Pain Hypersensitivity as Sign of Central Sensitization in Unilateral Epicondylalgia: A Blinded, Controlled Study. Clin. J. Pain 25, 555 (2009).
- Park, H. B., Gwark, J.-Y., Im, J.-H. & Na, J.-B. Factors Associated With Lateral Epicondylitis of the Elbow. Orthop. J. Sports Med. 9, 23259671211007734 (2021).
- Singh, H. P. & Watts, A. C. BESS patient care pathway: Tennis elbow. Shoulder Elb. 15, 348–359 (2023).
- van Rijn, R. M., Huisstede, B. M. A., Koes, B. W. & Burdorf, A. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology 48, 528–536 (2009).
- Zhang, C., Jia, Z., Li, J., Wang, X. & Yang, S. Impact of lifestyle and clinical factors on the prognosis of tennis elbow. Sci. Rep. 14, 3063 (2024).
- Lee, S. H., Gong, H. S., Kim, S., Kim, J. & Baek, G. H. Is There a Relation Between Lateral Epicondylitis and Total Cholesterol Levels? Arthroscopy 35, 1379–1384 (2019).
- Otoshi, K. et al. Chronic hyperglycemia increases the risk of lateral epicondylitis: the Locomotive Syndrome and Health Outcome in Aizu Cohort Study (LOHAS). SpringerPlus 4, 407 (2015).
- Tennis Elbow (Lateral Epicondylitis) – OrthoInfo – AAOS. https://www.orthoinfo.org/en/diseases–conditions/tennis-elbow-lateral-epicondylitis/.
- Nirschl, R. P. & Ashman, E. S. Elbow tendinopathy: tennis elbow. Clin. Sports Med. 22, 813–836 (2003).
- Hennig, E. M. Influence of Racket Properties on Injuries and Performance in Tennis. Exerc. Sport Sci. Rev. 35, 62 (2007).
- Mohandhas, B. R. et al. Racquet string tension directly affects force experienced at the elbow: implications for the development of lateral epicondylitis in tennis players. Shoulder Elb. 8, 184–191 (2016).
- Yolaçan, H. & Güler, S. Effect of elbow carrying angle on lateral epicondylitis development. Medicine (Baltimore) 102, e35789 (2023).
- Day, J. M., Lucado, A. M. & Uhl, T. L. A COMPREHENSIVE REHABILITATION PROGRAM FOR TREATING LATERAL ELBOW TENDINOPATHY. Int. J. Sports Phys. Ther. 14, 818–829 (2019).
- Musculoskeletal Pain during the Menopausal Transition: A Systematic Review and Meta-Analysis. 8842110 (2020) doi:10.1155/2020/8842110.
- Blumer, J. Arthralgia of menopause – A retrospective review. Post Reprod. Health 29, 95–97 (2023).
- Karjalainen, T. & Buchbinder, R. Is it time to reconsider the indications for surgery in patients with tennis elbow? Bone Jt. J. 105-B, 109–111 (2023).
- Ikonen, J. et al. Persistent Tennis Elbow Symptoms Have Little Prognostic Value: A Systematic Review and Meta-analysis. Clin. Orthop. 480, 647–660 (2022).
- Santiago, A. O., Rios-Russo, J. L., Baerga, L. & Micheo, W. Evidenced-Based Management of Tennis Elbow. Curr. Phys. Med. Rehabil. Rep. 9, 186–194 (2021).
- Saroja, G., Leo, A. & venkata sai, P. DIAGNOSTIC ACCURACY OF PROVOCATIVE TESTS IN LATERAL EPICONDYLITIS. Int. J. Physiother. Res. 2, 815–823 (2014).
- Coombes, B. K., Bisset, L. & Vicenzino, B. A new integrative model of lateral epicondylalgia. Br. J. Sports Med. 43, 252–258 (2009).
- Heales, L. J., Broadhurst, N., Mellor, R., Hodges, P. W. & Vicenzino, B. Diagnostic Ultrasound Imaging for Lateral Epicondylalgia: A Case–Control Study. Med. Sci. Sports Exerc. 46, 2070 (2014).
- Elsayed, M., Hafez, M. R. M. & Ibrahim, M. A. H. Ultrasound with shear wave elastography in diagnosis and follow-up of common extensor tendinopathy in cases with lateral epicondylitis: a cross-sectional analytic study. Egypt. J. Radiol. Nucl. Med. 53, 236 (2022).
- Lee, M. H. et al. Utility of sonographic measurement of the common tensor tendon in patients with lateral epicondylitis. AJR Am. J. Roentgenol. 196, 1363–1367 (2011).
- Toit, C. du, Stieler, M., Saunders, R., Bisset, L. & Vicenzino, B. Diagnostic accuracy of power Doppler ultrasound in patients with chronic tennis elbow. Br. J. Sports Med. 42, 872–876 (2008).
- Bachta, A. et al. Ultrasonography versus magnetic resonance imaging in detecting and grading common extensor tendon tear in chronic lateral epicondylitis. PloS One 12, e0181828 (2017).
- Obradov, M. & Anderson, P. G. Ultra sonographic findings for chronic lateral epicondylitis. JBR-BTR Organe Soc. R. Belge Radiol. SRBR Orgaan Van K. Belg. Ver. Voor Radiol. KBVR 95, 66–70 (2012).
- Torp-Pedersen, T., Torp-Pedersen, S. & Bliddal, H. Diagnostic value of ultrasonography in epicondylitis. Ann. Intern. Med. 136, 781–782 (2002).
- Toprak, U. et al. Common extensor tendon thickness measurements at the radiocapitellar region in diagnosis of lateral elbow tendinopathy. Diagn. Interv. Radiol. Ank. Turk. 18, 566–570 (2012).
- Arslan, S. et al. Diagnostic Performance of Superb Microvascular Imaging and Other Sonographic Modalities in the Assessment of Lateral Epicondylosis. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 37, 585–593 (2018).
- De Zordo, T. et al. Real-time sonoelastography of lateral epicondylitis: comparison of findings between patients and healthy volunteers. AJR Am. J. Roentgenol. 193, 180–185 (2009).
- Zhu, B., You, Y., Xiang, X., Wang, L. & Qiu, L. Assessment of common extensor tendon elasticity in patients with lateral epicondylitis using shear wave elastography. Quant. Imaging Med. Surg. 10, 211–219 (2020).
- Xu, Y. et al. Platelet-Rich Plasma Has Better Results for Long-term Functional Improvement and Pain Relief for Lateral Epicondylitis: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Am. J. Sports Med. 52, 2646–2656 (2024).
- Hohmann, E., Tetsworth, K. & Glatt, V. Corticosteroid injections for the treatment of lateral epicondylitis are superior to platelet-rich plasma at 1 month but platelet-rich plasma is more effective at 6 months: an updated systematic review and meta-analysis of level 1 and 2 studies. J. Shoulder Elbow Surg. 32, 1770–1783 (2023).
- Hardy, R. et al. To Improve Pain and Function, Platelet-Rich Plasma Injections May Be an Alternative to Surgery for Treating Lateral Epicondylitis: A Systematic Review. Arthroscopy 37, 3360–3367 (2021).
- Majidi, L., Khateri, S., Nikbakht, N., Moradi, Y. & Nikoo, M. R. The effect of extracorporeal shock-wave therapy on pain in patients with various tendinopathies: a systematic review and meta-analysis of randomized control trials. BMC Sports Sci. Med. Rehabil. 16, 93 (2024).
- Clark, T. et al. Arthroscopic Versus Open Lateral Release for the Treatment of Lateral Epicondylitis: A Prospective Randomized Controlled Trial. Arthrosc. J. Arthrosc. Relat. Surg. 34, 3177–3184 (2018).
- OrthoGlobe. Open and Arthroscopic Treatment of Lateral Epicondylitis (Tennis Elbow) Open and Arthroscopic Treatment of Lateral Epicondylitis (Tennis Elbow). Ortho Globe https://orthoglobe.org/open-and-arthroscopic-treatment-of-lateral-epicondylitis-tennis-elbow/ (2024).