This blog was completed as part of a post-graduate sports physiotherapy paper at Otago University, New Zealand.
Key Words: Exercise technique, movement patterns, exercise as medicine
Physios are in a unique position to fight the burden of disease. But are we doing our part when considering the statistics of what conditions have the highest burden?
Among musculoskeletal disorders, lower back pain (LBP) ranks the highest in terms of disability-adjusted life years (DALYs-millions). LBP was ranked 9th in 2021, with other musculoskeletal disorders taking the 19th ranking with scores of 70.2 and 49.2 DALYs respectively according to analysis for the Lancet Global Burden of Disease Study 2021, published this year. Compared to other non-communicable diseases, the burden of LBP is less than ischaemic heart disease and stroke but ranked higher than other MSK conditions (Figure 1). This highlights the crucial role of physiotherapy in reducing the burden of non-communicable diseases like back pain.
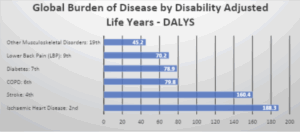
Figure 1: Global burden of disease by disability adjusted life years
Recently, when attending an educational session hosted by an experienced physio, they proposed some particular movement strategies as “optimal”. I was struck by some of the language used, insinuating that people may become injured if they cannot perform movements in a certain way or that by observing movement, we might be able to determine an optimal strategy based on pre-defined expectations. Some caveats about exceptions to the rules were added, but how might a less informed population be able to reason with those caveats, and how may this influence their actions? This confronted me, and I wondered if I was experiencing cognitive dissonance, so I wanted to explore my beliefs to see how solid the footings were.
In my role as a weightlifting coach and a physio, there aren’t many things I enjoy more than analysing someone’s movement technique frame by frame, especially when you can see immediate performance benefits. However, something I have become more aware of in my career is the influence of my language and communication style, as well as how the information is received. I have also become more aware of just how poor the state of physical activity is. I have come to find that an alarming number of people cite fear of injury as the reason for not engaging in physical activity (Huebschmann et al., 2011). Often, the fears surrounding injury/pain are reported to have come from their healthcare providers (Gardner et al., 2017; Setchell et al., 2017). Thus, we could have the potential to create an avoidance behaviour for physical activity as a whole by over-emphasising the minutiae of technique in our dealings with patients experiencing an episode of pain.
As sports physiotherapists, our goal should be to see the person before the athlete and to promote physical activity wherever possible. This is even more critical when dealing with weight-unrestricted athletes, who, although they are athletes, can still show other risk factors associated with poor cardiometabolic health status (Guo, Zhang, Wang, Guo, & Xie, 2013; Mansell, Blackburn, Arnold, & Arnason, 2011). Physical activity is a potent tool in our arsenal for combatting these risk factors, so we should do everything possible to keep it on the table in our communication. It has even been suggested that in the context of athletes with lower back pain, we should do more to promote physical activity when, intuitively, you would think they already do plenty of physical activity (O’Sullivan, O’Sullivan, Gabbett, & O’Keeffe, 2019).
The number needed to treat with an intervention to meet internationally recommended activity levels at 12 months was as low as 12 in one study (Orrow, Kinmonth, Sanderson, & Sutton, 2012). As physiotherapists, we spend a significant amount of time with clients by comparison with GPs, and we are often tasked with helping people get back to their preferred activity, so we are well placed to initiate conversations surrounding physical activity levels. Being aware of our potential to instill negative beliefs that may lead to avoidance will allow us to maximise our potential to foster positive behaviours. This knowledge strengthens the basis for a saying I heard recently during a motivational interviewing educational session that “people need a damn good listening to rather than a damn good talking to “, as well as a similar statement that “language is the load that strengthens the mind”.
Author Kyle Turvey BHSc Physiotherapy – Bachelor of Health Science (Physiotherapy), PGDipSEM – Post Graduate Diploma in Sport and Exercise Medicine
Instagram @kyle_potentia_physio
Private Practice musculoskeletal/sports physiotherapist and clinic director at Potentia Physiotherapy, Auckland, New Zealand.
The author declares no competing interests.
References
Gardner, T., Refshauge, K., Smith, L., McAuley, J., Hübscher, M., & Goodall, S. (2017). Physiotherapists’ beliefs and attitudes influence clinical practice in chronic low back pain: a systematic review of quantitative and qualitative studies. J Physiother, 63(3), 132-143. doi:10.1016/j.jphys.2017.05.017
Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. (2024). Lancet, 403(10440), 2133-2161. doi:10.1016/s0140-6736(24)00757-8
Guo, J., Zhang, X., Wang, L., Guo, Y., & Xie, M. (2013). Prevalence of metabolic syndrome and its components among Chinese professional athletes of strength sports with different body weight categories. PLoS ONE, 8(11), e79758. doi:10.1371/journal.pone.0079758
Huebschmann, A. G., Crane, L. A., Belansky, E. S., Scarbro, S., Marshall, J. A., & Regensteiner, J. G. (2011). Fear of injury with physical activity is greater in adults with diabetes than in adults without diabetes. Diabetes Care, 34(8), 1717-1722. doi:10.2337/dc10-1801
Mansell, K., Blackburn, D., Arnold, B., & Arnason, T. (2011). Prevalence of metabolic syndrome among college football linemen. Can J Diabetes, 35(5), 497-502. doi:10.1016/s1499-2671(11)80005-5
O’Sullivan, K., O’Sullivan, P. B., Gabbett, T. J., & O’Keeffe, M. (2019). Advice to athletes with back pain-get active! Seriously? Br J Sports Med, 53(6), 324-325. doi:10.1136/bjsports-2018-099670
Orrow, G., Kinmonth, A. L., Sanderson, S., & Sutton, S. (2012). Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. Bmj, 344, e1389. doi:10.1136/bmj.e1389
Setchell, J., Costa, N., Ferreira, M., Makovey, J., Nielsen, M., & Hodges, P. W. (2017). Individuals’ explanations for their persistent or recurrent low back pain: a cross-sectional survey. BMC Musculoskelet Disord, 18(1), 466. doi:10.1186/s12891-017-1831-7