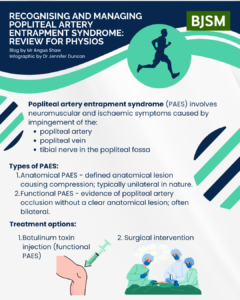
Popliteal Artery Entrapment Syndrome (PAES), first described in 1965, involves neuromuscular and ischemic symptoms caused by pathologic impingement of the popliteal artery (PA), with or without the involvement of the popliteal vein, and tibial nerve in the popliteal fossa (1). Compression commonly involves the medial head of the gastrocnemius muscle and may be congenital or acquired through muscular hypertrophy (2). PAES has an estimated incidence of 0.17% to 3.5%, with approximately 85% of cases affecting males, predominantly athletes under 30 years old (2).
The median delay in diagnosis is 12 months, with reports of misdiagnosis lasting up to 15 years due to the young age of patients, lack of atherosclerotic risk factors, and similarity to other lower limb conditions. If undiagnosed, it can progress to chronic complications, including arterial occlusion, critical limb ischemia, aneurysm formation, or even amputation (3).
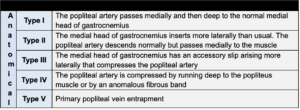
Types of PAES
- Anatomical PAES: Involves a defined anatomical lesion causing compression and occlusion of the popliteal artery. Is typically unilateral in nature (2, 3).
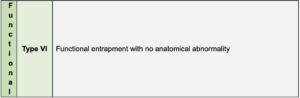
- Functional PAES (FPAES): Characterised by evidence of PA occlusion without a clear anatomical lesion. Often bilateral, with the medial head of the gastrocnemius muscle contributing to crowding in the popliteal fossa. Functional compression occurs in 30% to 50% of the general population and can affect both trained and untrained individuals (2, 3). The plantaris muscle is another overlooked culprit for vascular compression.
Figure 1. Popliteal Artery Entrapment Classification System (3).
Signs and Symptoms
PAES typically presents with (typically one of or a combination of the following)
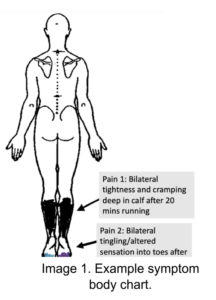
- Calf cramping & tightness/fullness, swelling, paraesthesia into the feet and toes, coldness, or loss of distal pulses with exertion.
- Ache deep in the calf after exercise/calf loading or prolonged postures.
- Key aggravators: calf-loading exercises, uphill walking, stair climbing, hiking, running, sustained plantarflexion, or prolonged standing.
- In some cases, pressing a car accelerator may also provoke symptoms.
Differential Diagnosis
PAES can mimic conditions like chronic exertional compartment syndrome (CECS) and other vascular or musculoskeletal disorders. Distinguishing between anatomical and functional PAES requires further investigation, as clinical symptoms alone are insufficient. Other lower limb vascular conditions to consider include External Iliac Artery Endofibrosis and deep vein thrombosis (2, 3, 4).
Figure 2. Differential diagnosis and clinical features of exertional leg pain. Adapted and modified from Hislop et al. 2014 (2)

Physio-Specific Assessment
- Subjective: History of exercise or posture-induced calf pain with matching symptoms.
- Objective:
- Observation: Redness, swelling, increased tone or discoloration of the calf/foot at rest or post-exertion.
- Gait: Increased plantarflexion tendencies during push-off.
- Functional Tests: Progression from double-leg calf raises to single-leg hops and running/incline treadmill walking while monitoring symptoms.
- Palpation: Evaluate atypical muscle bulk in the popliteal fossa during prone plantarflexion contraction.
- Pedal Pulse: Check at rest and during sustained plantarflexion, using auscultation if needed.
Note: Clinical examination alone cannot diagnose PAES.
Referral for further investigations: Patients should be referred to a sports physician for diagnostic testing, including:
- Provocative Doppler Ultrasound: Pre-and post-exercise to assess blood flow (2).
- Ankle-Brachial Index (ABI): Evaluates peripheral vascular disease but has limitations in PAES.
- Functional MR Angiogram: Provides detailed vascular imaging.
- Compartment Pressure Testing: May co-exist with PAES which can blur the clinical picture, especially as intercompartmental pressures may not correlate with symptoms (5).
Treatment Options
- Non-Operative:
- Botulinum Toxin A (BTA): First-line treatment for FPAES. Injected into the culprit musculature under electromyographic guidance. Proposed benefits include:
- Muscle paralysis to alleviate dynamic arterial occlusion.
- Localised muscle atrophy to create more space for vessels.
- Possible vasodilation of the popliteal artery (2, 6).
- Success rates exceed 50%, with risks lower than surgery. Treatment typically involves 1–3 sessions, with potential follow-ups. Case reports highlight successful return to sport with strategic BTA use in season (7).
- Botulinum Toxin A (BTA): First-line treatment for FPAES. Injected into the culprit musculature under electromyographic guidance. Proposed benefits include:
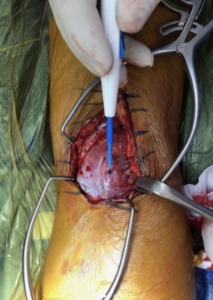
- Surgical Intervention:
- Surgery depends on the PAES subtype and symptoms. Early intervention focuses on musculotendinous release, while advanced cases may require arterial bypass (3, 8).
- For Anatomical PAES, procedures include myotomy of the medial head of the gastrocnemius, re-routing of the artery, and additional decompression for complex cases.
- For Functional PAES, options include myotomy, fasciotomy, plantaris muscle excision, and other decompressive techniques.
- Long-term recurrence in FPAES may result from fibrosis around the neurovascular bundle.
Image 2. Intraoperative image of my right leg during a MHGM myotomy, with removal measuring 15cm long and 4cm wide.
Post-Treatment Considerations
- Validated methods for assessing post-operative outcomes are lacking (6). Some studies measure return-to-sport rates or changes in exercise ABI. Long-term follow-up may be necessary to monitor recurrence and address fibrosis-related issues (6).
- My clinical opinion is that creatine supplementation and the use of blood flow restriction training should not be used in those with PAES. Careful re-loading of the calf musculature post-op e.g., only doing seated calf raises with modified rep-ranges may reduce the chance of muscular redevelopment post-op.
Conclusion
- Recognising PAES: PAES is an important differential diagnosis for chronic exertional leg pain. It is commonly missed, leading to delays in diagnosis and treatment.
- Management: Understanding the appropriate referral pathways and treatment options is crucial when presented with a PAES patient. Consider Botulinum Toxin A for functional cases and surgery for anatomical cases, with careful rehab post-op to prevent recurrence.
- For a concise audio summary of PAES, click here to listen to podcast on Spotify.
Author
Mr. Angus Shaw – Physiotherapist at Complete Physio London. Special interest in the assessment and diagnosis of chronic exertional lower leg pain. Angus brings a unique perspective on the topic of chronic exertional leg pain having had personal experience with the condition (4 x FPAES operations and 11 x fasciotomies for CECS).
No Competing Interests
References
-
- Turnipseed WD. Popliteal entrapment syndrome. Journal of Vascular Surgery. 2002 May 1;35(5):910-5. doi:10.1067/mva.2002.125364.
- Hislop M, Tierney P, Murray D. Functional popliteal artery entrapment syndrome: a review. J Sports Med. 2014;48(5):435-43. doi:10.1177/0363546514559282.
- Hameed M, Teh J, Sinha S. Popliteal artery entrapment syndrome: diagnosis and management. Br J Sports Med. 2018;52(7):459-64. doi:10.1136/bjsports-2016-096421.
- Brewer RB, Gregory AJM. Chronic Lower Leg Pain in Athletes: A Guide for the Differential Diagnosis, Evaluation, and Treatment. Sports Health. 2012;4(2):121-127. doi:10.1177/1941738111426115
- Zimmermann WO, Behrens M, Fischer A, et al. Intracompartmental pressure and exercise pain. Transl J ACSM. 2018;3(9):125-30. doi:10.1249/TJX.0000000000000072.
- Lovelock T, Firth J, Hamilton B. Functional PAES: diagnosis and management. Int J Sports Med. 2021;42(3):205-11. doi:10.1055/a-1211-5206.
- Murphy M, Brennan M, Rankin A. Botulinum toxin injection in functional PAES. Phys Ther Sport. 2017;25:92-6. doi:10.1016/j.ptsp.2016.12.008.
- Bradshaw S, O’Neill D, Fitzpatrick A. Popliteal artery entrapment syndrome. Cardiovasc Diagn Ther. 2021;11(5):1234-42. doi:10.21037/cdt-21-44.