Introduction:
Whether it’s from a collision on the basketball court, a fall on the ice, or a hard tackle on the football pitch; concussion is a serious injury that can disrupt an athlete’s season and result in a prolonged absence from their sport. Commonly reported acute symptoms include headache, nausea, dizziness, memory impairment and confusion. The underlying cerebral damage can present as measurable neurological deficits in cognition, balance and reaction time (1).
The challenge faced by medical staff treating sports players with concussion often goes beyond the initial management of their medical symptoms. There is the added component of comprehensively assessing when the player can be reintroduced into training and return to sport. The relative lack of objective measurements in concussion assessment is a particular challenge (2). Particularly at the elite level, sports teams and the athlete themselves may be eager for a swift return to sports, however a premature return can result in an increased chance of symptom relapse (3). In contrast, a more conservative approach in the post-concussion period could potentially lead to longer absences from sport than necessary. In any case, a clinician having access to quality concussion assessment tools will prove invaluable when making such decisions.
Assessing Concussion and Vestibulo-Ocular Motor Screening:
In the acute post-concussion stage, the Sport Concussion Assessment Tool 6 (SCAT6) is used to investigate concussion (4), and beyond 72 hours it is recommended that Sport Concussion Office Assessment Tool (SCOAT6) is used to assist individualised management plans (5). When assessing recovery, according to the 2023 consensus statement (6), there has been a move towards incorporating vestibular and oculomotor function, alongside symptoms and examination findings, as seen in SCOAT6. The vestibular-ocular deficit is an established neurological finding after concussion in both adults and adolescents (7). A section of the SCOAT6 includes vestibular-ocular motor screening (VOMS), where smooth eye pursuits, saccades, Vestibulo-ocular reflex (VOR) and Visual Motion Sensitivity (VMS) are all tested to see if symptoms are reproduced [Figure 1]. The test is carried out by a trained examiner, with the only equipment needed being a metronome and a tongue depressor with a size 14 font printout attached. If any of the symptoms are reproduced, then the patient will be asked to rank symptom severity on a scale of 1-10, the examiner may also note down the patient’s performance on each of the tests. Symptom severity scores and performance notes can then be compared to baseline values if available. A video overview of the assessment can be found here (8).
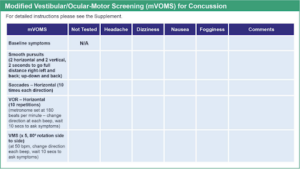
Figure 1 – Modified Vestibular/Ocular-Motor Screening section of the Sport Concussion Office Assessment Tool. (9)
This traditional VOMS assessment does come with some downsides. As the symptom severity reporting is subjective, there is the potential for patients to inaccurately report their symptoms or downplay symptoms to accelerate their return to sport. It is also worth noting that the examiners interpretation of the patients’ performance is also subjective and prone to variation between assessments and different examiners. Furthermore, there may also be discrepancies in the way the test is carried out from one assessment or examiner to the next.
Importantly, any single assessment tool should not be used in isolation by a clinician to make a recovery assessment, and instead a holistic approach should be taken when deciding if an athlete is ready to train or ready to return to competition (6).
How the test works:
In recent years, computerised vestibulo-ocular and ocular-motor assessment tools have started to enter mainstream concussion care. One such tool leverages virtual reality (VR) technology to objectively measure the VOMS assessment (Neuroflex.io, Canada) (10). The innovative VR headset is plugged into a PC or laptop, the associated software is loaded and patient details are entered [Figure 2]. Once the headset is fitted comfortably, it has sensors within that detect even the smallest of eye movements.

Figure 2 – Headset connected to laptop.
A series of eight tests are conducted, each of which produces a detailed numerical data set that shows metrics such as eye vergence, saccades, directional accuracy amongst others. These metrics are reported because post-concussion, there is a deficit in the ability to control eye movement and focus on objects within a patient’s visual field. Furthermore, there is a deficit in the compensatory movements of the eyes in relation to the head, when fixating on moving or fixed objects (7).
The assessment can be conducted when the athlete is healthy as a baseline and then post-concussion for comparison. The 8 tests are described as follows:
Smooth pursuit [Head free]
This task aims to test the ability of the individual to smoothly track a moving target [Figure 3]. The head-free test is a representation of real life movement including visual, vestibular and neck proprioception.
Metrics reported: Mean Vergence, Mean Error and Head contribution in both horizontal and vertical planes.

Figure 3 – Computer screen display that the assessor can see during the test. Shows the graphic that the patient can see, their eye movements and the percentage of the test that has elapsed.
Smooth pursuit [Head fixed]
The subject attempts to follow a target moving in sinusoidal motion with their head stationary. This test better tests isolated oculomotor functions and is better suited to subjects with cervical issues. The target trajectory is randomised between trials to avoid the training effect.
Metrics reported: Mean Vergence, Mean Error and Number of Saccades.
Acute Visual VOR [Horizontal]
The vestibulo-ocular reflex (VOR) causes movement of the eyes in a direction opposite to the direction of movement of the head, thus maintaining clear vision and helping to fixate on the target during head movement. This test will evaluate the ability of the subject to successfully maintain clear vision while focusing on a target during side to side head movement.
Metrics reported: Mean Vergence, Gain left and right.
Acute Visual VOR [Vertical]
This task tests the VOR during movement of the head in the vertical plane. As with the horizontal VOR test, if the VOR does not produce the eye movements required, the patient may report dizziness and blurred vision, which will need to be noted down by the examiner.
Metrics reported: Mean Vergence, Gain up and down.
Saccades
The saccadic system allows rapid, conjugate movements that shift the gaze from one point in the visual field to another. This task tests the system by producing targets randomly within the field of vision of ± 25 degrees. Deficits can be detected in specific parts of the visual field (e.g, only on the right side).
Metrics reported: Mean Vergence, Mean Latency and Acquisition Error.
Anti-saccades
The subject is asked to look at a target in the centre of the screen and then a red X appears to the right or left of the target. The subject is asked not to look at the X and instead look at a point which is an equal distance from the target in the opposite direction from the red X. This tests inhibition and visual map orientation which are functions of the visual cortex.
Metrics reported: Mean Vergence, Mean Latency, Acquisition Error and Directional Accuracy.
Optokinetic Nystagmus
This task involves keeping the head fixed while the subject is instructed to follow a point in a moving field of dots. The test aims to induce visual slip in the horizontal and vertical planes and at variable velocities, which in turn causes nystagmus.
Metrics reported: Mean Vergence, Gain (left, right up and down).
Spontaneous Nystagmus
Spontaneous nystagmus is a rapid, involuntary movement of the eyes without vestibular, visual or cognitive stimuli. The subject is instructed to look at a flashed target that disappears and then continue looking in the same orientation for a few seconds. This tests the spontaneous saccade frequency (tremor frequency).
Metrics reported: Mean Tremor Frequency, Tremor velocity and Average Drift.
Case study – Aspetar Hospital:
The Aspetar Hospital, a FIFA Medical Centre of Excellence located in Doha, is currently in its first year of utilising the Neuroflex VOMS tool for baseline concussion screening. The sports medicine department has incorporated it as a standard test within its athlete screening programme. In Qatar, the athletes from all the national clubs will come to Aspetar for their initial and yearly medical assessment, meaning baseline VOMS scores are regularly updated. In the event of a sports related concussion the athlete will be monitored with the VR headset, and the post-concussion VOMS scores can be compared to their most recent baseline. Post-concussion testing is usually done weekly, or as needed for specific clinical indications. Due to the precise numerical data generated from these tests, the clinicians have an accurate data-set that can help inform rehabilitation decisions and their return to sport assessment.
The test itself is generally well tolerated by athletes, as the test duration is relatively short and the headset is usually found to be comfortable. The overall impression is that athletes enjoy the test due to the ‘game’ element of it. One concern I heard from an athlete prior to completing their baseline assessment was the fear of feeling dizzy and nausea from wearing the headset and doing the virtual reality test. Sickness symptoms from virtual reality head-mounted displays is an established side effect (11). However, risk factors associated with sickness as a side effect include prolonged exposure time and frequent use (11) , which is the opposite of the way the virtual reality headset is utilised for VOMS assessments.
When the assessment is put into practice, it is vital that the athlete understands what each test requires them to do. If the athlete did not understand, or is not compliant with the constraints of any of the tests, the assessor must restart that test so that the results are valid. For example, the assessor must be vigilant and spot if an athlete is moving their head during a head-fixed test.
Summary:
Computerised VR vestibulo-ocular and ocular-motor assessment has proven to be a convenient tool with itsit’s ease of use and ability to generate detailed numerical data. Its comfortable design and quick testing time means athletes can be tested at regular intervals so baseline values are available for comparison after an injury. Nevertheless these tests should be used in conjunction with other tools and clinical judgement to assess an athlete’s progress rather than being used as a standalone test.

Authors:
- Dillan Dhanak, Bsc (Hons), University College London Medical School, MBBS
- Ayan Nadeem, Northwest School Of Medicine, Pakistan, MBBS
- Fekih Akram, PT,OMPT, Aspetar Hospital
- Prof. Louis Holtzhausen, MBChB Ph.D, Aspetar Hospital – Chief of Sports Medicine, founder and director of the Aspetar Sports Concussion Program
References:
- Giza CC, Kutcher JS. An Introduction to Sports Concussions. Contin Lifelong Learn Neurol. 2014 Dec;20(6 Sports Neurology):1545–51.
- Jb T, Bl B, L N, T M, Lc P, Ar M, et al. Role of biomarkers and emerging technologies in defining and assessing neurobiological recovery after sport-related concussion: a systematic review. PubMed [Internet]. [cited 2024 Aug 30]; Available from: https://pubmed.ncbi.nlm.nih.gov/37316184/
- Carson JD, Diep D, Baker C, Kraft SA, Kuwahara N, Garel A, et al. Relapse of concussion symptoms in the context of premature return to learn and return to play. 2022 Mar 1 [cited 2024 Aug 17]; Available from: https://www.cfp.ca/content/68/3/e87.short
- Echemendia RJ, Brett BL, Broglio S, Davis GA, Giza CC, Guskiewicz KM, et al. Introducing the Sport Concussion Assessment Tool 6 (SCAT6). 2023 Jun 1 [cited 2024 Aug 17]; Available from: https://bjsm.bmj.com/content/57/11/619
- Patricios JS, Schneider GM, Ierssel J van, Purcell LK, Davis GA, Echemendia RJ, et al. Beyond acute concussion assessment to office management: a systematic review informing the development of a Sport Concussion Office Assessment Tool (SCOAT6) for adults and children. 2023 Jun 1 [cited 2024 Aug 17]; Available from: https://bjsm.bmj.com/content/57/11/737
- Patricios JS, Schneider KJ, Dvorak J, Ahmed OH, Blauwet C, Cantu RC, et al. Consensus statement on concussion in sport: the 6th International Conference on Concussion in Sport–Amsterdam, October 2022. 2023 Jun 1 [cited 2024 Aug 17]; Available from: https://bjsm.bmj.com/content/57/11/695
- Treleaven D, Lamontagne A, Grilli L, Friedman D, Gagnon I. Altered Oculomotor and Vestibulo-ocular Function in… : The Journal of Head Trauma Rehabilitation. [cited 2024 Aug 17]; Available from: https://journals.lww.com/headtraumarehab/fulltext/2024/07000/altered_oculomotor_and_vestibulo_ocular_function.15.aspx
- What is the VOMS? | UPMC Sports Medicine Concussion Program [Internet]. 2016 [cited 2024 Aug 17]. Available from: https://www.youtube.com/watch?v=XlA_wJAMBmg
- Medicine BPGL and BA of S and E. Sport Concussion Office Assessment Tool 6 (SCOAT6). 2023 Jun 1 [cited 2024 Aug 17]; Available from: https://bjsm.bmj.com/content/57/11/651
- Neuroflex [Internet]. [cited 2024 Aug 19]. Home. Available from: https://neuroflex.io/
- 11. Saredakis D, Szpak A, Birckhead B, Keage HAD, Rizzo A, Loetscher T. Factors Associated With Virtual Reality Sickness in Head-Mounted Displays: A Systematic Review and Meta-Analysis. Front Hum Neurosci. 2020 Mar 31;14:96.