Authors: Larissa Rodrigues Souto, Danilo De Oliveira Silva, and Marcella Ferraz Pazzinatto.
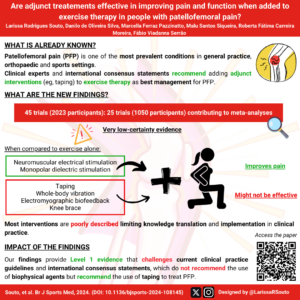
In this blog we discuss the findings of our recent study published in BJSM that evaluated the effectiveness of adjunct treatments combined with exercise therapy compared to exercise therapy alone in people with patellofemoral pain (PFP) and appraised the quality of the intervention description in PFP randomised controlled trials (RCTs).
Why is this study important?
Patellofemoral pain (PFP) is a complex multifactorial condition characterised by pain around or behind the patella during activities that load the patellofemoral joint.(1) Its annual prevalence is about 23% in adults and 29% in adolescents.(2) PFP has a poor prognosis with 57% not recovered 8 years post-treatment.(3)
Exercise therapy is the key treatment for PFP,(4) as a single intervention or combined with multimodal approaches.(1) Clinical guidelines recommend combining exercise therapy with adjunct treatments such as patellar taping and biofeedback to improve clinical symptoms in PFP.(1, 5) No recent systematic review has explored whether individual adjunct treatments add value to exercise therapy. This can guide clinicians to offer the most efficient management for patients with PFP.
Our findings can inform upcoming PFP clinical practice guidelines and international consensus statements. Additionally, we appraised the quality of intervention descriptions in RCTs, which is crucial to ensure knowledge translation and appropriate implementation in clinical practice.
How did the study go about this?
We searched seven databases for studies that assessed the effectiveness of adjunct treatments combined with exercise therapy compared to exercise therapy alone for patients with PFP on self-reported measures of pain and function.
Where there were two or more studies that were sufficiently similar, meta-analyses were performed. Pooled analyses were created for the following groups of interventions combined with exercise therapy: (1) neuromuscular electrical stimulation (NMES), (2) monopolar dielectric diathermy, (3) knee taping; (4) whole-body vibration, (5) knee brace and (6) electromyographic biofeedback. All interventions had exercise therapy alone as the comparator. All the pooled analyses were performed considering the outcomes evaluated at short-term (< 3 months).
We appraised the quality of the intervention descriptions, for each intervention (adjunct treatment and exercise therapy), and assessed the risk of bias using the Template for Intervention Description and Replication (TIDieR) checklist and the Cochrane Risk of Bias 2, respectively. The quality of intervention description was classified as ‘good’, ‘moderate’ or ‘poor’ and, the risk of bias was classified as ‘low risk’, ‘some concerns’ or ‘high risk’. The certainty of evidence from each meta-analysis was assessed by the GRADE approach.
What did the study find?
We included 45 RCTs (n=2023 participants), with 25 RCTs (n=1050 participants) contributing to meta-analyses. Our analyses indicated very-low certainty evidence that NMES and monopolar dielectric diathermy combined with exercise leads to small and large improvements in self-reported pain when compared to exercise alone in the short-term, respectively. For self-reported pain and function, very low-certainty evidence indicates that knee taping, whole body vibration, electromyographic biofeedback and knee brace combined with exercise do not differ from exercise alone in the short-term.
Except for five trials, which had moderate-quality descriptions for both interventions, and one trial, which had moderate-quality and good-quality descriptions for adjunct treatment and exercise therapy, respectively, the overall quality of intervention description was generally poor. Regarding risk of bias assessment, we rated 10 outcomes as ‘some concerns’ and 67 outcomes as ‘high risk of bias’.
What are the key take-home points?
1) Very low-certainty evidence suggests that in the short term, NMES or monopolar dielectric diathermy, combined with exercise, improves self-reported pain in people with PFP compared to exercise therapy alone, with small and large effects, respectively.
2) Very low-certainty evidence suggests that knee taping, whole-body vibration, electromyographic biofeedback and knee brace do not add value to exercise therapy.
3) Most interventions are poorly described limiting knowledge translation and implementation in clinical practice.
4) Our findings provide level 1 evidence that challenges current clinical practice guidelines and international consensus statements, which recommend that biophysical agents (e.g., electrical stimulation, monopolar dielectric diathermy) should not be used in people with PFP and that knee taping should be used alongside exercise therapy.
References
- Barton CJ, Lack S, Hemmings S, Tufail S, Morrissey D. The ‘Best Practice Guide to Conservative Management of Patellofemoral Pain’: incorporating level 1 evidence with expert clinical reasoning. Br J Sports Med. 2015;49(14):923-34.
- Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, et al. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS One. 2018;13(1):e0190892.
- Lankhorst NE, van Middelkoop M, Crossley KM, Bierma-Zeinstra SM, Oei EH, Vicenzino B, et al. Factors that predict a poor outcome 5-8 years after the diagnosis of patellofemoral pain: a multicentre observational analysis. Br J Sports Med. 2016;50(14):881-6.
- Crossley KM, Stefanik JJ, Selfe J, Collins NJ, Davis IS, Powers CM, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med. 2016;50(14):839-43.
- Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, et al. Patellofemoral Pain. J Orthop Sports Phys Ther. 2019;49(9):Cpg1-cpg95.