Keywords: anterior cruciate ligament healing; Cross Bracing Protocol; anterior cruciate ligament injury; non-surgical; patient-reported outcomes
Why is this study important?
Anterior cruciate ligament (ACL) rupture often results in poor long-term outcomes such as decreased sport participation, early onset of knee osteoarthritis, persistent pain, and impaired long term quality of life, irrespective of treatment. Current management strategies for ACL rupture are based on the assumption that the ACL has limited healing capacity. A recent analysis of a randomised controlled trial found evidence of ACL healing on magnetic resonance imaging (MRI) in at least one-third of patients with ACL rupture, at 2 years after being randomised to treatment with rehabilitation and optional delayed surgery (1). ACL healing on 2 year MRI was associated with better patient-reported outcomes compared to a non-healed ACL, or management with ACL surgery. These findings give rise to the opportunity for new interventions that aim to facilitate non-surgical healing of ACL rupture. The Cross Bracing Protocol (CBP) is a novel treatment involving a knee brace and rehabilitation that aims to facilitate ACL healing (2).
This blog summarises a recent paper reporting ACL healing and outcomes from the first people with ACL rupture managed with this novel bracing protocol (2).
How did the study go about this?
We investigated clinical outcomes of the first 80 consecutive patients with acute ACL rupture who were managed with the CBP in clinical practice (2). The CBP consists of 12 weeks of knee bracing coupled with physiotherapist-supervised exercise-based rehabilitation. For the first 4 weeks the knee brace is locked at 90 degrees flexion, followed by weekly adjustments to the brace allowing incremental increases in knee range-of-motion, with unrestricted range-of-motion achieved by week 10. Weight bearing was allowed whilst braced, within the available range-of-motion. Patients were prescribed an anticoagulant for the first 8 weeks to mitigate the risk of deep vein thrombosis (DVT) (2). At 12 weeks, the brace was removed and patients underwent a 12-week MRI and clinical review (Figure 1). Patient reported outcomes were collected at a median 12 months after ACL injury.
We analysed MRIs obtained at 3 months and 6 months after commencing the CBP, to assess evidence of ACL healing (continuity, thickness and length of the ACL) following management with the CBP (2). We also compared 12 month patient-reported outcomes (including knee function, knee-related quality of life and return to pre-injury sport rates) and knee laxity tests, between people with more or less signs of ACL healing on 3 month MRI (more healing = a continuous and thickened ACL; less healing = a continuous and thinned/elongated ACL, or a discontinuous ACL) (2).
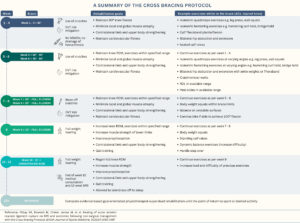
Figure 1. A summary of the Cross Bracing Protocol.
DVT, Deep vein thrombosis; MRI, Magnetic resonance imaging; NSAIDs, Non-steroidal anti-inflammatory drugs; RDL, Romanian deadlift; ROM, Range of motion.
What did the study find?
Evidence of ACL healing on 3-month MRI was observed in 72 out of 80 (90%) patients who were managed with the CBP (n=40 (50%) had a continuous thickened ACL, and n=32 had a continuous but thinned or elongated ACL) (Figure 2). Of the eight ACLs that remained ruptured, 6 had attached to surrounding structures (the lateral wall and/or posterior cruciate ligament) (2). We also found that participants with more ACL healing reported better knee function and knee-related quality of life after 12 months compared to those with less ACL healing. This group also had reduced knee laxity and more people returned to pre-injury sport compared with the group with less ACL healing. Eleven (14%) patients re-injured their ACL (Figure 3) (2).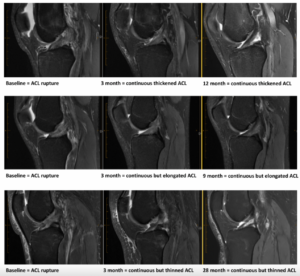
Figure 2. Evidence of ACL healing on MRI at two follow-up time points.
ACL, Anterior cruciate ligament
What are the key take-home points?
Findings of this study provide further evidence that the ACL has the potential to heal and the high healing rate observed on MRI suggests that the CBP could play a facilitative role in ACL healing. The variability in the patterns of ACL healing seen on MRI suggests there may be a spectrum of ACL healing. Although a continuous thickened ACL on 3-month MRI was associated with the best patient outcomes, those with a continuous and thinned/elongated ACL also reported very good patient reported outcomes, on average. It is not yet known how outcomes compare following the CBP compared to other management strategies. We are performing a comparative effectiveness randomised controlled trial to address this knowledge gap and inform clinical practice.

Figure 3. Key findings
ACL, Anterior cruciate ligament; IQR, Interquartile range; MRI, magnetic resonance imaging; QOL, Quality of life.
References:
(1) Filbay SR, Dowsett M, Chaker Jomaa M, et al. Healing of acute anterior cruciate ligament rupture on MRI and outcomes following non-surgical management with the Cross Bracing Protocol. Br J Sports Med. 2023;57(23):1490-1497. doi:10.1136/bjsports-2023-106931
Authors:
Meike van Haeringen, Tom Cross, Stephanie Filbay.
Correspondence:
A/Prof Stephanie Filbay, Centre for Health Exercise and Sports Medicine, Department of Physiotherapy, University of Melbourne, Victoria, Australia.
Email: stephanie.filbay@unimelb.edu.au
X = @stephfilbay
References
- Filbay SR, Roemer FW, Lohmander LS, et al. Evidence of ACL healing on MRI following ACL rupture treated with rehabilitation alone may be associated with better patient-reported outcomes: a secondary analysis from the KANON trial. British Journal of Sports Medicine 2023;57(2):91-98. doi: 10.1136/bjsports-2022-105473
- Filbay SR, Dowsett M, Jomaa MC, et al. Healing of acute anterior cruciate ligament rupture on MRI and outcomes following non-surgical management with the Cross Bracing Protocol. British Journal of Sports Medicine 2023:bjsports-2023-106931. doi: 10.1136/bjsports-2023-106931