Don’t lose your nerve with the ulnar nerve: A guide to working up entrapment neuropathies.
Introduction: What is Ulnar Nerve Entrapment?
Ulnar nerve entrapment neuropathies commonly present to MSK and orthopaedics clinics, with patient’s reporting (pins and needles, paraesthesia, or muscle weakness) that fits a typical distribution. Unpicking the site of compression of the nerve, during a focussed clinical exam, can help clinicians to decide on what work up (imaging, EMG, injection therapy or orthopaedic interventions are needed). We discuss the key clinical tests to use as part of your work, the common imaging findings, and treatment options for ulnar nerve entrapment syndromes.
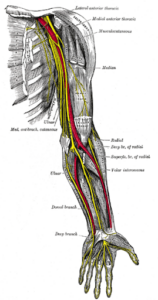
Getting to grips with the ulnar nerve
Ulnar nerve entrapment is the second most common entrapment neuropathy in the upper limb, (after carpal tunnel syndrome). It commonly occurs at two main anatomical landmarks one at the elbow (cubital tunnel syndrome) and one at the wrist (Guyon’s canal syndrome).
- Cubital tunnel syndrome – has a reported incidence of 30/100,00 (1)
- Incidence of Guyon’s canal syndrome unclear due to lack of population studies.
- Ulnar nerve entrapment neuropathies are reported to be twice as common in middle aged males compared to females (2)
- It has been reported to be common in exercising patients and athletes (cycling, baseball, golfers, weightlifters) and construction workers (24).
Common causes of entrapment neuropathies, include trauma, anatomical variations, functional positions, and compressive lesions.

The Ulnar nerve: Nerve roots and & function
| Spinal roots |
|
| Ulnar nerve course |
|
| Sensory functions |
|
| Motor functions |
|
 (3)
(3)
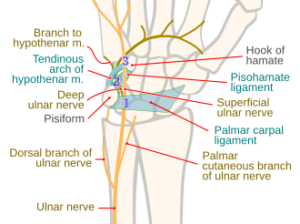
The anatomy of Cubital tunnel and Guyon’s Canal
- Cubital tunnel: space between posterior and transverse bands of the medial collateral ligament (deep) and Obsbourne’s ligament where the ulnar nerve enters the forearm
- Guyon’s canal: formed by four borders, volar carpal ligament (roof), transverse carpal ligament (floor), hook of hamate (radial border) and pisiform (ulnar border). The canal is further subdivided into three zones, which cause different clinically relevant symptoms (4):
- Zone 1: dual motor and sensory deficit
- Zone 2: isolated motor deficit
- Zone 3: isolated sensory deficit
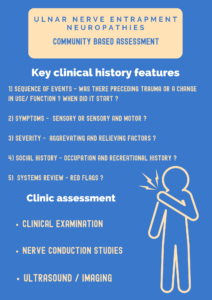
The clinical history: working up red flags and common compression sites.
Once red flag conditions have been ruled out (cervical compression, brachial compression, systemic features, and masses). The diagnosis of ulnar nerve entrapment syndromes can be made from 5 S features in the clinical history, alongside the clinical exam.
History
In the clinical history, there are three broad considerations to think about before moving to take a more focussed history.
- Does the patient have any red flag features?
- Weight loss, night pain, pain unrelated to movement, neck mass, axillary mass, generalised muscle weakness, bilateral symptoms
- Have I ruled out a more central compression in the neck or brachial plexus?
- Eg, Thoracic outlet syndrome
3) Have I considered systemic disorders? (5)
- Eg, neuromuscular disorders eg, ALS
Take a focussed history using the 5S focused history:

Examination
| Guyon’s canal syndrome (5) | Cubital tunnel syndrome | |
| Physical examination |
|
|
|
|
|
| Motor examination |
|
|
| Sensory examination |
|
|
| Vascular examination |
|
|
| Differentiators between Guyon’s canal and Cubital tunnel syndrome |
|
|
Imaging
MSK Imaging can be considered when there is a suspicion of an underlying compressive lesion. This usually starts with ruling out proximal site before going distal (Cervical Spine > Thoracic outlet > Brachial plexus > Cubital Tunnel > Guyon’s Canal).

Electrodiagnostic testing
Whilst a suspected diagnosis of ulnar nerve entrapment neuropathies can be made on clinical examination and history, there are some cases where further studies nerve conduction studies (NCS) and electromyogram (EMG) may be useful (7). This is when there is diagnostic uncertainty or where you may need to locate the exact location of the entrapment to aid injection targets or surgical planning. In practical terms this is most important if you need to distinguish between:
-
C8 radiculopathy vs a peripheral ulnar nerve neuropathy
-
Nerve entrapment at the medial epicondyle vs cubital tunnel
-
The level of compression at the Guyon’s canal
Nerve conduction studies (NCS) analyse large myelinated sensory and motor fibres, in controlled conditions. Characteristic changes to summated action potentials of sensory (SNAPs) and motor muscle fibres (CMAPs), can help to determine the site of compression.
|
Lesion distal to Guyon’s canal |
Lesion at the level of the elbow |
|
|
Key Ultrasound findings of Cubital Tunnel and Guyon’s Canal Entrapment
Ultrasound is a highly effective tool used for the assessment of ulnar nerve neuropathies, alongside the characterisation of symptoms (5 S approach). It allows for dynamic assessment of nerve morphology, measurements of the affected and unaffected areas of the nerve can be assessed with movement & functional compression. MSK Ultrasound can also uses to deliver diagnostic and therapeutic steroid injections or nerve hydro-disection procedures (9).
|
Guyon’s Canal Syndrome |
Cubital Tunnel Syndrome |
|
|
|
Ultrasound findings in cubital tunnel syndrome |
Sensitivity (%) |
Specificity (%) |
|
Cross sectional area cut off for ulnar nerve |
||
|
> 8.95mm (15) |
93.8 |
88.3 |
|
>9mm (16) |
84 |
80 |
|
>9.5mm (17) |
100 |
80 |
|
>10mm (18) (19) |
82-88 |
72-88 |
|
Distance from Medial epicondyle to nearest surface of Ulnar nerve at full elbow extension |
||
|
<0.53cm (20) |
71.4 |
90.7 |
|
MSK imaging |
Description |
|
|
Axial MRI STIR sequence images at the level of the cubital tunnel Finding: Perineural oedema of the ulnar nerve |
|
|
Axial MRI STIR sequence images at the level of the cubital tunnel Finding: The Ulna nerve is enlarged with a bright appearance. |
|
|
Ultrasound images in the transverse plane depicting the cubital tunnel Findings: Ultrasound findings showing a cross sectional area of 10mm2 upper end of normal. Findings: The second image shows an avulsion fracture of the medial epicondyle causing ulna nerve impingement symptoms. Dynamic ultrasound |
|
|
Axial MRI T1W image Finding Normal ulna nerve – visualised at Guyon’s canal. |
Management options
Ulnar nerve neuropathies can be managed in 3 ways:
Conservative management
Mild symptoms that do not severely impact quality of life can be managed conservatively (splinting & activity modification) (25). Think about the 5S’s history you took for the patient with a particular focus on the ‘Social’ part of the history which considered the occupation and recreational history. Tailored advice, focussed rehabilitation and biomechanics adjustments can be delivered on a case-by-case basis depending on the precipitating and aggravating factors. For example, for a cyclist where you might suspect the cycling as being the causative factor underling their symptoms, you may recommend a change in handlebars or grip to help alleviate symptoms.
Minimally invasive treatments
Minimally invasive treatments involve corticosteroid or dextrose injections which have shown variable efficacy rates in patients. This may depend on the severity of the neuropathy.
|
Authors |
Type of study |
Comparison of injection |
Participants (n=) |
Outcomes |
Main take away points from the study |
|
Chen et al (26) |
Prospective, randomized, double-blind, controlled trial |
Single perineural injection with 5 mL Dextrose 5% with water compared to 3 mL corticosteroid (triamcinolone acetonide, 10mg/mL) mixed with 2 mL normal saline |
36 |
|
|
|
Vanveen et al (21) |
Randomised double blinded study |
40mg methylprednisolone acetate and 10mg lidocaine hydrochloride compared to placebo |
55 |
|
|
|
Kaplan et al (22) |
Randomised double blinded study |
5cc 5% dextrose injection compared to normal saline |
40 |
|
|
Surgical treatment
In cases where conservative or minimally invasive techniques have proven to be ineffective, surgical treatment may be indicated. There are a variety of surgical techniques, which have the unifying aim of nerve decompression, and the two most common interventions are simple decompression and decompression with transposition of the ulnar nerve.
Surgical treatment is recommended in cases where:
-
Conservative and non-invasive treatment trials have led to no improvement.
-
Serious compression of the ulnar nerve
-
Muscle weakness/damage from nerve compression
Surgical outcome tends to be good, but the degree of compression must be considered. In severe compression, (muscle wasting) or loss of nerve function symptoms may remain after surgery. Since nerve recovery is slow, it may take a while to see the surgical outcomes.
The aim of surgical treatment is to relieve pressure on the ulnar nerve so that it is no longer compressed and able to glide freely through the full range of motion.
|
Cubital tunnel syndrome surgical techniques |
|||
|
Operation |
Cubital tunnel release for mild/moderate nerve compression where the nerve does not slide out from the medial epicondyle on elbow flexion. |
Ulnar nerve anterior transposition |
Medial epicondylectomy |
|
Technique |
Cubital tunnel ligament (Osborne’s ligament) roof cut and divided so tunnel size is increased and less pressure on the nerve. |
There nerve is moved anterior to the medial epicondyle. Three variations:
|
Removal of part of the medial epicondyle to prevent nerve compression on bony ridge on elbow flexion. |
A review identified no statistically significant difference between simple decompression and transposition surgeries in terms of clinical and neurophysiological improvement, but a higher number of wound infections was associated with transposition surgeries (23). Post-surgical recovery often required splinting for 3-6 weeks alongside a rehabilitation programme.
Surgery to treat ulnar nerve compression at the wrist involves either removing the cause of construction or opening the Guyon’s canal. As with decompression at the cubital tunnel, it may take a while to see the surgical outcome, with possible incomplete recovery in older patients with long-term compression and some muscle wasting/weakness being irreversible.
Conclusion
-
Ulnar nerve entrapment commonly occurs at two anatomical landmarks: Guyon’s canal and the Cubital tunnel.
-
A detailed clinical history using the 5S framework and the scratch collapse test can be used in clinic to localise an ulnar nerve peripheral neuropathy.
-
Nerve conduction studies can help to grade the degree and site of neuropathy.
-
Ultrasound features such as – enlarged cross sectional area, dynamic subluxation or evidence of compressive lesions can help to diagnose the condition.
Authors
Dr Osama Munajjed
Senior House Officer
Imperial College Healthcare Trust
Miss Geethana Yogarajah
5th year medical student, University of Cambridge
Dr Rifat Hassan
Foundation Year 1 doctor
Norfolk & Norwich University Hospitals
@RifatHassan_
Dr Preena Patel
Consultant Musculoskeletal and Paediatric Radiologist
MSK Lead (Imaging)
Luton & Dunstable University Hospital
Dr Irfan Ahmed
Locum Consultant in Musculoskeletal, Sport & Exercise Medicine, Addenbrooke’s Hospital
Twitter @ExerciseIrfan
Mr Niel Kang
Consultant Trauma & Orthopaedic Surgeon
Cambridge University Hospitals NHS Trust
Affiliate Assistant Professor
Clinical school of medicine, University of Cambridge
Education and Careers Committee
British Orthopaedic Association
Twitter @kangstagram77
No relevant conflicts of interests or relevant disclosures declared by any of the authors.
credit statement: Conceptualization: O.M., G.Y., I.A. and N.K.; Data curation: R.H. and O.M.; Supervision: I.A. and N.K.; MSK imaging: P.P.; Writing – original draft: O.M. and G.Y.; Writing – review & editing: O.M., G.Y., R.H., P.P., I.A. and N.K.
References:
-
Osei DA, Groves AP, Bommarito K, Ray WZ. Cubital Tunnel Syndrome: Incidence and Demographics in a National Administrative Database. Neurosurgery. 2016 Dec 27;80(3):417–20.
-
Mondelli M, Giannini F, Ballerini M, Ginanneschi F, Martorelli E. Incidence of ulnar neuropathy at the elbow in the province of Siena (Italy). Journal of the Neurological Sciences [Internet]. 2005 Jul 15 [cited 2023 Mar 27];234(1-2):5–10. Available from: https://pubmed.ncbi.nlm.nih.gov/15993135/
-
Wikipedia. Ulnar nerve entrapment [Internet]. Available from: https://en.wikipedia.org/wiki/Ulnar_neuropathy#/media/File:Nerves_of_the_left_upper_extremity.gif
-
Maroukis BL, Ogawa T, Rehim SA, Chung KC. Guyon Canal: The Evolution of Clinical Anatomy. The Journal of Hand Surgery. 2015 Mar;40(3):560–5.
-
Earp BE, Floyd WE, Louie D, Koris M, Protomastro P. Ulnar Nerve Entrapment at the Wrist. Journal of the American Academy of Orthopaedic Surgeons. 2014 Nov;22(11):699–706.
-
Ramage JL, Varacallo M. Anatomy, Shoulder and Upper Limb, Hand Guyon Canal. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534814/
-
Bains S, Rocha Cabrero F. Electrodiagnostic Evaluation of Ulnar Neuropathy. [Updated 2022 Oct 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564408/
-
Elhassan, Bassem MD; Steinmann, Scott P. MD. Entrapment Neuropathy of the Ulnar Nerve. Journal of the American Academy of Orthopaedic Surgeons 15(11):p 672-681, November 2007
-
Mezian K, Jačisko J, Kaiser R, Machač S, Steyerová P, Sobotová K, et al. Ulnar Neuropathy at the Elbow: From Ultrasound Scanning to Treatment. Frontiers in Neurology [Internet]. 2021 May 14 [cited 2023 Apr 2];12:661441. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8160369/
-
Choi SJ, Ahn JH, Ryu DS, Kang CH, Jung SM, Park MS, et al. Ultrasonography for nerve compression syndromes of the upper extremity. Ultrasonography. 2015 Jan 13;34(4):275–91.
-
Guyon’s Canal Syndrome [Internet]. www.evidencesportandspinal.com. Available from: https://www.evidencesportandspinal.com/Injuries-Conditions/Hand/Hand-Issues/Guyon-s-Canal-Syndrome/a~286/article.html
-
Chang KV, Wu WT, Han DS, Özçakar L. Ulnar Nerve Cross-Sectional Area for the Diagnosis of Cubital Tunnel Syndrome: A Meta-Analysis of Ultrasonographic Measurements. Archives of Physical Medicine and Rehabilitation [Internet]. 2018 Apr 1;99(4):743–57. Available from: https://pubmed.ncbi.nlm.nih.gov/28888384/
-
Beekman R, Visser LH, Verhagen WI. Ultrasonography in ulnar neuropathy at the elbow: A critical review. Muscle & Nerve. 2011 Apr 11;43(5):627–35.
-
Kerasnoudis A, Tsivgoulis G. Nerve Ultrasound in Peripheral Neuropathies: A Review. Journal of Neuroimaging. 2015 May 21;25(4):528–38.
-
Kim JH, Won SJ, Rhee WI, Park HJ, Hong HM. Diagnostic Cutoff Value for Ultrasonography in the Ulnar Neuropathy at the Elbow. Annals of Rehabilitation Medicine. 2015;39(2):170.
-
Rayegani SM, Raeissadat SA, Kargozar E, Rahimi-Dehgolan S, Loni E. Diagnostic value of ultrasonography versus electrodiagnosis in ulnar neuropathy. Medical Devices: Evidence and Research. 2019 Feb;Volume 12:81–8.
-
Hamdy M, Hafez AE, Mohamed AK & FA. Diagnostic role of neuromuscular ultrasound in cubital tunnel syndrome. International Journal of Clinical Rheumatology [Internet]. 2020 Jan 8 [cited 2023 Oct 14];14(6):288. Available from: https://www.openaccessjournals.com/articles/diagnostic-role-of-neuromuscular-ultrasound-in-cubital-tunnel-syndrome-13130.html
-
Ayromlou H, Tarzamni MK, Daghighi MH, Pezeshki MZ, Yazdchi M, Sadeghi-Hokmabadi E, et al. Diagnostic Value of Ultrasonography and Magnetic Resonance Imaging in Ulnar Neuropathy at the Elbow. ISRN Neurology [Internet]. 2012 [cited 2020 Jul 20];2012:1–6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3409534/pdf/ISRN.NEUROLOGY2012-491892.pdf
-
Volpe A, Rossato G, Bottanelli M, Marchetta A, Caramaschi P, Lisa Maria Bambara, et al. Ultrasound evaluation of ulnar neuropathy at the elbow: correlation with electrophysiological studies. Rheumatology. 2009 Sep 1;48(9):1098–101.
-
Lee GJ, Park D. Ultrasonographic Findings of the Ulnar Nerve Following Elbow Flexion in Patients with Cubital Tunnel Syndrome. Pain Medicine. 2020 Jun 28;21(11):2684–91.
-
vanVeen KEB, Alblas KCL, Alons IME, Kerklaan JP, Siegersma MC, Wesstein M, et al. Corticosteroid injection in patients with ulnar neuropathy at the elbow: A randomized, double-blind, placebo-controlled trial. Muscle & Nerve. 2015 Jun 18;52(3):380–5.
-
Başak Mansız-Kaplan, Barış Nacir, Secil Pervane-Vural, Olcay Tosun Meric, Burcu Duyur Çakıt, Hakan Genç. Effect of Perineural Dextrose Injection on Ulnar Neuropathy at the Elbow: A Randomized, Controlled, Double-Blind Study. Archives of Physical Medicine and Rehabilitation. 2022 Nov 1;103(11):2085–91.
-
Caliandro P, La Torre G, Padua R, Giannini F, Padua L. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2016 Nov 15;11(11):CD006839. doi: 10.1002/14651858.CD006839.pub4. PMID: 27845501; PMCID: PMC6734129.
-
Raut P, Jones N, Raad M, Kieffer W. Common peripheral nerve entrapments in the upper limb. Br J Hosp Med (Lond). 2022 Oct 2;83(10):1-11. doi: 10.12968/hmed.2022.0111. Epub 2022 Oct 30. PMID: 36322444.
-
Chen LC, Ho TY, Shen YP, Su YC, Li TY, Tsai CK, Wu YT. Perineural Dextrose and Corticosteroid Injections for Ulnar Neuropathy at the Elbow: A Randomized Double-blind Trial. Arch Phys Med Rehabil. 2020 Aug;101(8):1296-1303. doi: 10.1016/j.apmr.2020.03.016. Epub 2020 Apr 20. PMID: 32325164.