This is part 2 of 2 of a blog series on greening the curriculum. You can read part 1 by clicking here!

Picture by Keira Burton
When incorporating SHE into physiotherapy curriculums the barriers we have highlighted must be addressed. Not all students and graduates thought it was a good idea, and those that did were often concerned about workload and relevance. One way to ensure relevance would be to use it as a theme throughout the degree when covering more traditional topics. For example:
- Orthopaedics & musculoskeletal care (MSK)
Pathways have been developed to reduce the impact of MSK care on the environment [14]. - Non-communicable diseases
Links between air pollution and many health conditions exist, including COPD, asthma, hypertension, type 2 diabetes, and others [1, 2, 3, 10, 15, 17]. Management strategies for these conditions can have very different ecological impacts [6]. - Neurology
Links have been found between poor environmental conditions and certain diseases [8, 21]. This is a new area of research, so there is more to discover. - Biopsychosocial model (BPS)
Understanding that every aspect of a person’s experience happens within their environment is important but often missed. This links to access to green spaces and population health issues such as poor housing [7]. - Communicable diseases
The origin of diseases that put many people in hospital, can be traced back to our relationship with the planet and other animals [11]. - Communication about climate change
Signposting to resources such as the Talking Climate Handbook [18] could improve confidence in talking about these issues – an important step in creating change [9]. - Sustainable development goals (SDGs)
These goals represent many population health issues, none of which happen in isolation and all of which affect health [16].
This approach would require no separate module, minimising workload and ensuring relevance.
The other barrier – SHE not being a main priority in healthcare – must be addressed in several ways because it’s a complicated theme. Understanding the significant health impacts related to climate change may help students understand why SHE should be a priority. Using statements such as “Climate Change is the single biggest health threat facing humanity” [19, 20], will provide an evidence-based hook for engaging students in this subject. With so many impacts, how can this not be a priority?
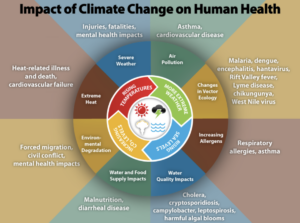
Infographic from Centres for Disease Control and Prevention
The concern that prioritising planetary health will negatively impact patient care must be addressed too. Patient care is paramount, but sustainability can also be a part of the equation [12]. If two treatments are likely to have similar outcomes for the patient, and one has less environmental impact, the “greener” one is the more appropriate [13]. Learning to factor this into clinical reasoning is an important skill.
It was common thinking that HCPs had no time to prioritise sustainability due to understaffing and underfunding. For years the health service in the UK has focussed on reacting to negative events and less so on preventing them. Changing this would result in fewer incidents and less pressure on the health system eventually, but it requires investment and long-term thinking [4]. If HCPs have the confidence to advocate for this, it may help to create a healthier and more sustainable society.

Picture by Markus Spiske
Key messages
- Physiotherapy students and physiotherapists have varied opinions on SHE. Some believe it should be encouraged, while others do not.
- Participants of this study were mainly concerned that SHE is not relevant to their practice as HCPs, that it would increase the workload for students and that it isn’t a priority in the healthcare setting.
- Addressing these concerns will be essential when universities incorporate SHE into their curriculums. Ideas have been explored here, although there are many other approaches [5]. Experimentation and conversation are always essential when investigating new ideas.

Author information
Millie Kent, Physiotherapist, University of Nottingham graduate, Twitter @MillieKentPT.
Acknowledgements
Ann Gates, Honorary Associate Professor University of Nottingham.
Fiona Moffatt, Associate Professor University of Nottingham.
Filip Maric, Associate Professor, UiT the Artic University of Norway.
Roger Kerry, Professor of Physiotherapy Education University of Nottingham.
References
- Committee on the Medical Effects of Air Pollutants. (2010). The Mortality Effects of Long-Term Exposure to Particulate Air Pollution in the United Kingdom. ISBN: 978-0-85951-685-3.
- Kelly F and Maynard R (2018). The Effects of Long-Term Exposure to Ambient Air Pollution on Cardiovascular Morbidity: Mechanistic Evidence A report by the Committee on the Medical Effects of Air Pollutants.
- Hansel NN, McCormack MC & Kim V (2016) The Effects of Air Pollution and Temperature on COPD, COPD: Journal of Chronic Obstructive Pulmonary Disease, 13:3, 372-379, DOI: 10.3109/15412555.2015.1089846
- Hewitt P. (2023). The Hewitt Review An independent review of integrated care systems. Available online: https://www.gov.uk/government/publications/the-hewitt-review-an-independent-review-of-integrated-care-systems [Accessed 20.04.23].
- Inspirational case-reports | Environmental Physiotherapy Asscociation. (n.d.). Available online: https://environmentalphysio.com/education/inspirational-case-reports/ [Accessed 15.03.23].
- Jeswani HK., and Azapagic A. (2019). Life cycle environmental impacts of inhalers. Journal of Cleaner Production, 237, 117733. https://doi.org/10.1016/J.JCLEPRO.2019.117733
- Lehman BJ., David DM, & Gruber JA. (2017). Rethinking the biopsychosocial model of health: Understanding health as a dynamic system. Social and Personality Psychology Compass, 11(8). https://doi.org/10.1111/SPC3.12328
- Louis S, Carlson AK, Suresh A, Rim J, Mays MA, Ontaneda D, & Dhawan A. (2023). Impacts of Climate Change and Air Pollution on Neurologic Health, Disease, and Practice. Neurology, 100(10), 474–483. https://doi.org/10.1212/WNL.0000000000201630
- Maibach E. (2021). Recognition and Commitment Every major public health victory of the last century has had effective communication at its heart.
- Maynard R. (2022). Cognitive decline, dementia and air pollution: a report by the Committee on the Medical Effects of Air Pollutants.
- Mishra J, Mishra P & Arora NK. (2021). Linkages between environmental issues and zoonotic diseases: with reference to COVID-19 pandemic. Environmental Sustainability 2021 4:3, 4(3), 455–467. https://doi.org/10.1007/S42398-021-00165-X
- Mortimer F, Isherwood J, Wilkinson A, & Vaux E. (2018). Sustainability in quality improvement: redefining value. Future Healthcare Journal, 5(2), 88. https://doi.org/10.7861/FUTUREHOSP.5-2-88
- National Institute of Health and Care Excellence (NICE). (2022). Asthma inhalers and climate change. ISBN: 978-1-4731-4750-8.
- Palstam A, Sehdev S, Barna S, Andersson M, & Liebenberg N. (2022). Sustainability in physiotherapy and rehabilitation. Orthopaedics and trauma Vol 36, Iss 5, Pages 279-283, ISSN 1877-1327, https://doi.org/10.1016/j.mporth.2022.07.005.
- Tiotiu AI, Novakova P, Nedeva D, Chong-Neto HJ, Novakova S, Steiropoulos P, & Kowal K. (2020). Impact of Air Pollution on Asthma Outcomes. International Journal of Environmental Research and Public Health 2020, Vol. 17, Page 6212, 17(17), 6212. https://doi.org/10.3390/IJERPH17176212
- United Nations. (2015). THE 17 GOALS | Sustainable Development. https://sdgs.un.org/goals
- Vallianou NG, Geladari EV, Kounatidis D, Geladari CV, Stratigou T, Dourakis SP, Andreadis EA, & Dalamaga M. (2021). Diabetes mellitus in the era of climate change. Diabetes & Metabolism, 47(4), 101205. https://doi.org/10.1016/J.DIABET.2020.10.003
- Webster R, & Marshall G. (2019). The #Talking Climate Handbook. How to have conversations about climate change in your daily life. Oxford: Climate Outreach. IBSN: 1865403334.
- World Health Organisation. (2021). 2021 WHO health and climate change global survey report. ISBN: 978-92-4-003850-9.
- World Health Organization. (2021, October 30). Climate change and health. https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health
- Zammit C, Torzhenskaya N, Ozarkar PD, & Calleja Agius J. (2021). Neurological disorders vis-à-vis climate change. Early Human Development, 155, 105217. https://doi.org/10.1016/J.EARLHUMDEV.2020.105217