Keywords: tendinopathy, intratendinous pressure
In this blog, we will explain the findings of our recent review published in BJSM on the potential role of intratendinous pressure in the pathogenesis of tendon pathology.
Why is this study important?
Tendinopathy is a major problem for athletes, accounting for about 30% of all overuse injuries. Despite strong advances in tendon research in recent decades, there is still a limited understanding of the underlying pathogenesis. The role of tissue pressure has not yet been considered a possible factor, although it has been associated with numerous other pathologies.
How did the study go about this?
This narrative review article encompassed an extensive literature search on four main aspects:
(1) the current understanding of intratendinous pressure in normal conditions
(2) the role of tissue pressure in the pathogenesis of other disorders that share structural similarities with tendons
(3) the relationship between compressive overload and tendon structure
(4) how structural changes in tendon pathology might alter intratendinous pressure
What did the study find?
- First, a conceptual framework was established defining five possible steps how intratendinous pressure could be involved in the development and progression of tendon pathology.
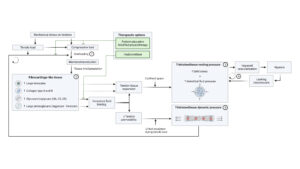
1.Compressive overload as pathogenic stimulus
It was found that compressive overload might be an initial trigger in the development of tendon pathology.
2.(Mal)adaptive tendon matrix remodeling
As tendon cells have the ability to detect and adapt to mechanical stimuli, overexpression of fibrocartilage-like tissue occurs as a result of compressive overload. This maladaptive remodelling is characterized by an increase of glycosaminoglycans (polysaccharides), proteoglycans (proteins), enlarged tenocytes and collagen type II and III.
3.Volume expansion induces an increase in intratendinous resting pressure
Every structure in our human body has a stable total tissue pressure of less than 15 mm Hg. This pressure is the sum of solid stress, ie, cells and extracellular matrix and interstitial fluid pressure, ie, free fluid. Pathological tendon changes, particularly the increase of glycosaminoglycans and proteoglycans with their bound fluid, could lead to an increase in intratendinous resting pressure, as the associated volume increase is resisted by enclosed sheaths (ie, endo- or epitenon).

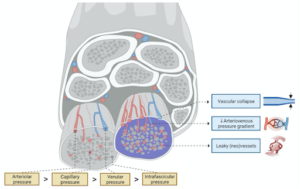
4.Increased intratendinous resting pressure impairs vascularisation
It is suggested that hypoxia (low oxygen levels) is a feature of tendon pathology. An increase in intratendinous resting pressure might drive this, as it could impair blood supply by inducing vascular collapse and lowering the arteriovenous pressure gradient. In addition, leakage of hypoxia-induced neovessels could also further increase interstitial fluid pressure, creating a vicious cycle.
5.Reduced permeability induces an increase in intratendinous dynamic pressure
Tendons experience lateral contraction during tensile loading, generating intratendinous dynamic pressure and consequently fluid excretion. This fluid pressure increases sharply when the permeability of the extracellular matrix decreases, because of higher resistance to fluid flow. Such a decrease in permeability typically occurs in tendon pathology due to the increase of water-retaining glycosaminoglycans and proteoglycans. Fluid can therefore be trapped inside the tendon matrix during tensile loading, resulting in an increase in intratendinous dynamic pressure. This also implies that for the same amount of tensile load, tendon cells will experience more pressure in tendon pathology than in healthy tendons, which again could create a vicious cycle.

- Second, it was identified how our novel theory might fit into the recognised continuum model of tendinopathy and correlate with its typical clinical manifestations (eg, load-related tendon pain).
- Third, potential treatment strategies were discovered that could restore intratendinous pressure to promote tendon healing. On the one hand, maladaptive tendon remodeling must be addressed. This can be done by reducing the amount of compressive load, but still exerting sufficient tensile forces on the tendon during rehabilitation. On the other hand, hyaluronidase also seems promising, as it breaks down the excess glycosaminoglycans of the extracellular matrix to pre-injury levels, releasing bound fluid and reducing both intratendinous resting and dynamic pressure.
What are the key take-home points?
- Intratendinous pressure might be an important contributor in tendinopathy. Our conceptual framework provides a coherent view of how intratendinous pressure could be involved in the development and progression of tendon pathology and helps to identify unexplored research opportunities.
- Maladaptive remodeling into fibrocartilage-like tissue could lead to both an increase in intratendinous resting and dynamic pressure, due to excess water-binding glycosaminoglycans and proteoglycans.
- An increase in intratendinous resting pressure could explain hypoxia in tendon pathology.
- An increase in intratendinous dynamic pressure might explain load-related tendon pain.
- Therapies aimed at inhibiting maladaptive remodeling (eg, modified physiotherapy) or reducing intratendinous pressure (eg, hyaluronidase) seem promising therapies that should be investigated.

Corresponding author:
Dr. Lauren Pringels, Department of Physical and Rehabilitation Medicine, Ghent University Hospital, Ghent, Belgium; Lauren.Pringels@Ugent.be
Reference:
Pringels L, Cook JL, Witvrouw E, et al. Exploring the role of intratendinous pressure in the pathogenesis of tendon pathology: a narrative review and conceptual framework. British Journal of Sports Medicine Published Online First: 02 November 2022. doi: 10.1136/bjsports-2022-106066