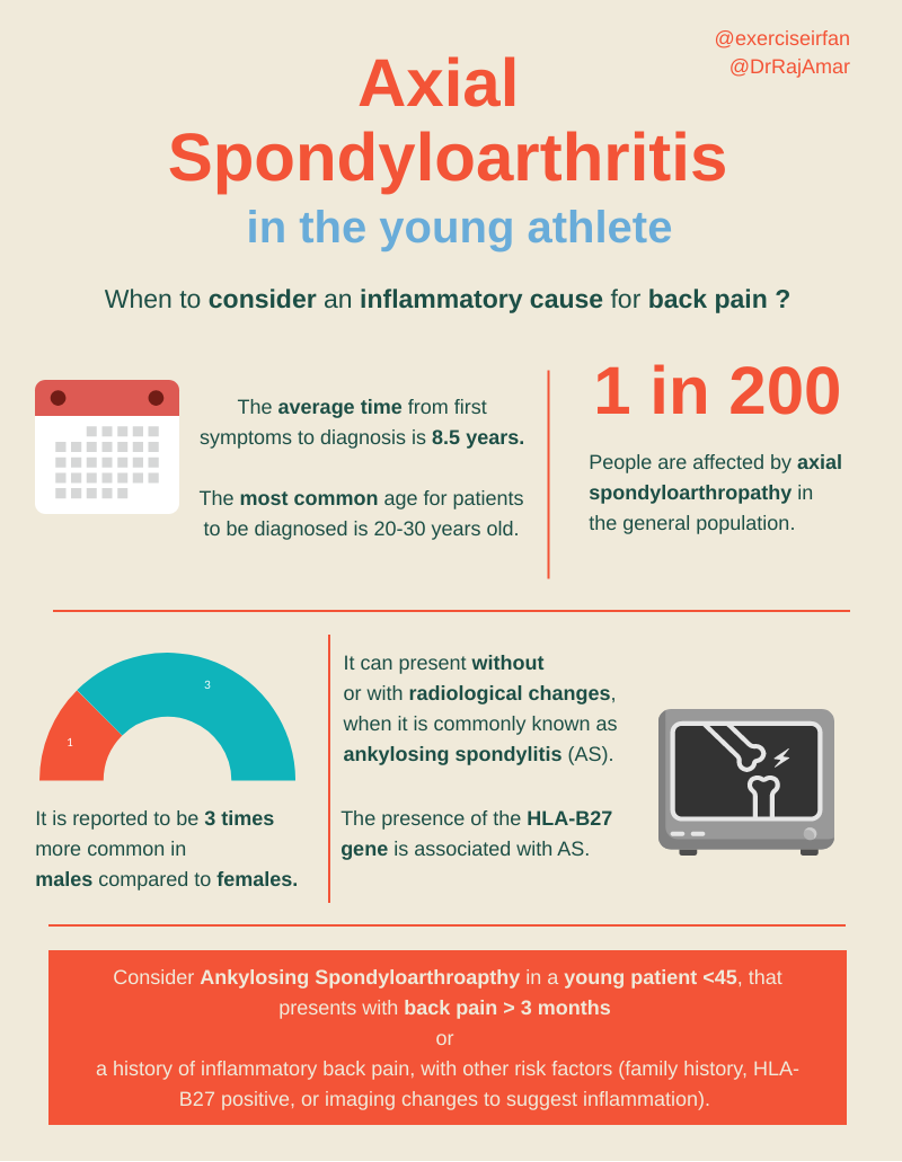
Axial Spondyloarthropathy (axSpA) a tricky diagnosis not to miss in the young athlete – part of the new UK SEM Trainee Blog Series
Back pain is a common complaint in the young adult athlete. This is often due to a combination of high training load, poor posture and biomechanical risk factors. However, there are a small number of patients where persistent back pain could be an early presentation of axial spondylarthritis (AxSpA). We discuss some of the key features of AxSpA that SEM clinicians should be aware of in order to help with early diagnosis and prompt rheumatology referral.
Axial Spondylarthritis – the need for speed in diagnosis.
AxSpA is a chronic, inflammatory disease that most often presents between the ages of 20-30 as arthritis in the spine and pelvis (1). For many athletes this may coincide with the peak of their sporting careers and can have a major impact on their quality of life (2), activities of daily living (3) and work (4). AxSpA, can either present with radiographic (previously known as ankylosing spondylitis (AS)) or non-radiographic disease.
Background
AxSpA affects 0.5% of the population (incidence – 1:200 people – UK data) (2) and has a male to female ratio of 3:1. However, wider use of MRI is now identifying the condition earlier in women (5). AxSpA is a difficult diagnosis to make in young athletes, given its relatively high prevalence and common presentation of musculoskeletal back pain in this group. The average time to diagnosis from first symptoms is 8.5 years (UK -data) (3).
Key features of inflammatory back pain include:
- Insidious onset
- Early morning stiffness
- Improvement with exercise
- Other associated inflammatory medical conditions: inflammatory bowel disease, psoriasis, uveitis (anterior). (4)
- Family history of AxSpA
It is also important to rule out other more serious presentations such as cauda equina syndrome (4).
There is a significant overlap between AxSpA symptoms and other types of back pain in this age group that may include growing pains, mechanical back pain, diffuse idiopathic skeletal hyperostosis (DISH), disc prolapse or myogenic (muscle related pain).
Athlete specific factors
The young adult athlete is often balancing sports training alongside other academic or life responsibilities, and back pain is therefore relatively common. A diagnosis of inflammatory arthritis can have major consequences for their sports aspirations and life after competition. It is therefore important that athletes presenting with possible signs of AxSpA are diagnosed early and seen by a specialist healthcare professional.
What investigations should I consider when looking for AxSpA
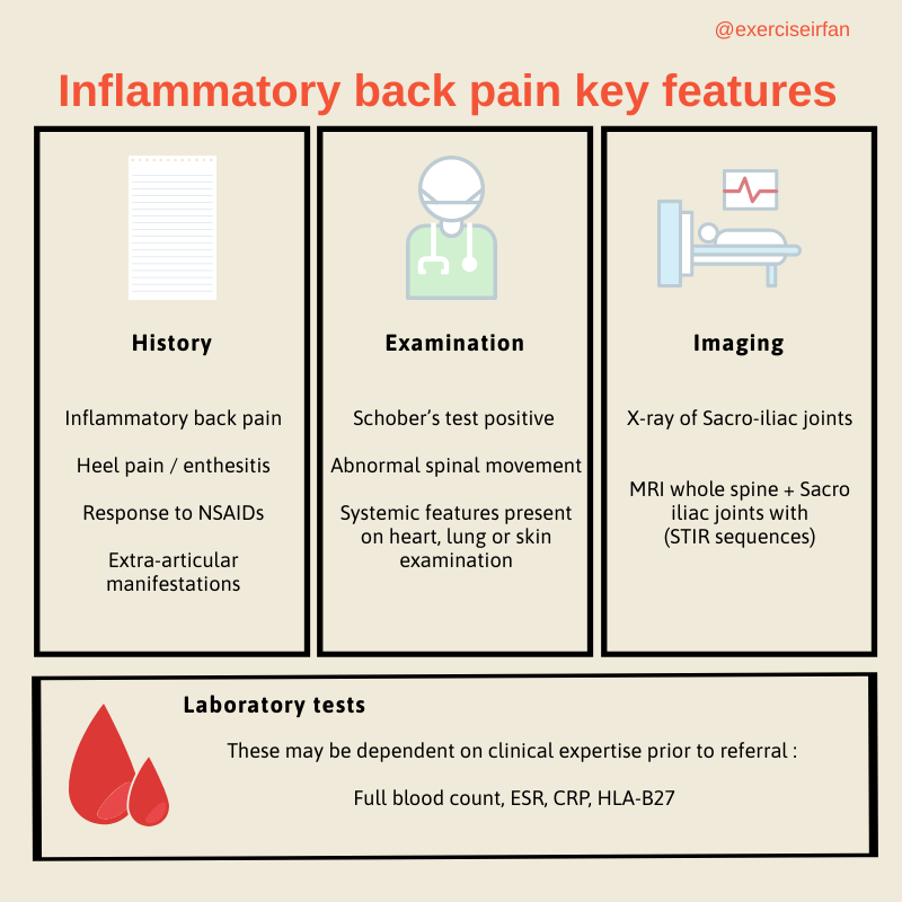
Although AxSpA is strongly associated with the HLA-B27 gene, this is not a specific diagnostic test. Making a diagnosis often involves a combination of history, physical examination, laboratory and radiographic tests.
NICE does not recommend routine use of inflammatory markers or X-ray outside of secondary care and patients should be referred to rheumatology if the clinical suspicion is high.
The National Axial Spondyloarthritis Society (NASS) have launched numerous educational resources (www.actonaxialspa.com) for healthcare professionals in order to try and reduce time to diagnosis. Further, the Royal National Hospital for Rheumatic Diseases have created a simple online checklist to help decide when chronic back pain may suggest AxSpA (http://www.spadetool.co.uk/).

If AxSpA is suspected, consider early referral to rheumatology as timely management is crucial. With appropriate medication, physiotherapy and exercise, most patients with AS live a normal life expectancy, often with minimal disability.
Conclusion
- AxSpA is a chronic, inflammatory disease that affects young adults and can present with insidious onset back pain
- There is often a delay to diagnosis due to the non-specific nature of the symptoms,
- Suspicion of inflammatory back pain symptoms should prompt early referral to rheumatology
Authors names & affiliations
Raj Amarnani
Sports & Exercise Medicine, Imperial College Healthcare NHS Trust, London, United Kingdom
Irfan Ahmed
Sports & Exercise Medicine, Homerton University Hospital Foundation Trust, London, United Kingdom
Madhura Castelino
Rheumatology Department, University College London Hospitals NHS Foundation Trust, London, United Kingdom
Infographics: @Exerciseirfan
Competing Interests
Nil
References
- Sieper J, Braun J, Rudwaleit M, Boonen A, Zink A. Ankylosing spondylitis: an overview. Ann Rheum Dis [Internet]. 2002 Dec;61 Suppl 3:iii8-18. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12381506
- Society NAS. Facts & Figures [Internet]. NASS Website. 2021 [cited 2021 Aug 28]. Available from: https://nass.co.uk/about-as/as-facts-and-figures/
- Adshead R, Donnelly S, Knight P, Tahir H. Axial Spondyloarthritis: Overcoming the Barriers to Early Diagnosis-an Early Inflammatory Back Pain Service. Curr Rheumatol Rep [Internet]. 2020;22(10):59. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32808099
- Sieper J, Braun J, Dougados M, Baeten D. Axial spondyloarthritis. Nat Rev Dis Prim [Internet]. 2015 Dec 9;1(1):15013. Available from: http://www.nature.com/articles/nrdp201513
- National Institute For Health and Care Excellence. Spondyloarthritis in over 16s: diagnosis and management [Internet]. 2017 [cited 2021 Aug 28]. Available from: https://www.nice.org.uk/guidance/ng65
- Rudwaleit M, Haibel H, Baraliakos X, Listing J, Märker-Hermann E, Zeidler H, et al. The early disease stage in axial spondylarthritis: results from the German Spondyloarthritis Inception Cohort. Arthritis Rheum [Internet]. 2009 Mar;60(3):717–27. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19248087
- Lim CSE, Sengupta R, Gaffney K. The clinical utility of human leucocyte antigen B27 in axial spondyloarthritis. Rheumatology [Internet]. 2018 Jun 1;57(6):959–68. Available from: https://academic.oup.com/rheumatology/article/57/6/959/4211017
- Sheehan NJ. The ramifications of HLA-B27. JRSM [Internet]. 2004 Jan 1;97(1):10–4. Available from: http://jrsm.rsmjournals.com/cgi/doi/10.1258/jrsm.97.1.10
- Singh JA, Strand V. Spondyloarthritis is associated with poor function and physical health-related quality of life. J Rheumatol [Internet]. 2009 May;36(5):1012–20. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19369461
- Dagfinrud H, Kjeken I, Mowinckel P, Hagen KB, Kvien TK. Impact of functional impairment in ankylosing spondylitis: impairment, activity limitation, and participation restrictions. J Rheumatol [Internet]. 2005 Mar;32(3):516–23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15742446
- Boonen A. A review of work-participation, cost-of-illness and cost-effectiveness studies in ankylosing spondylitis. Nat Clin Pract Rheumatol [Internet]. 2006 Oct;2(10):546–53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17016480