What can athletes do to prevent themselves being exposed to muscle breakdown after exercise?
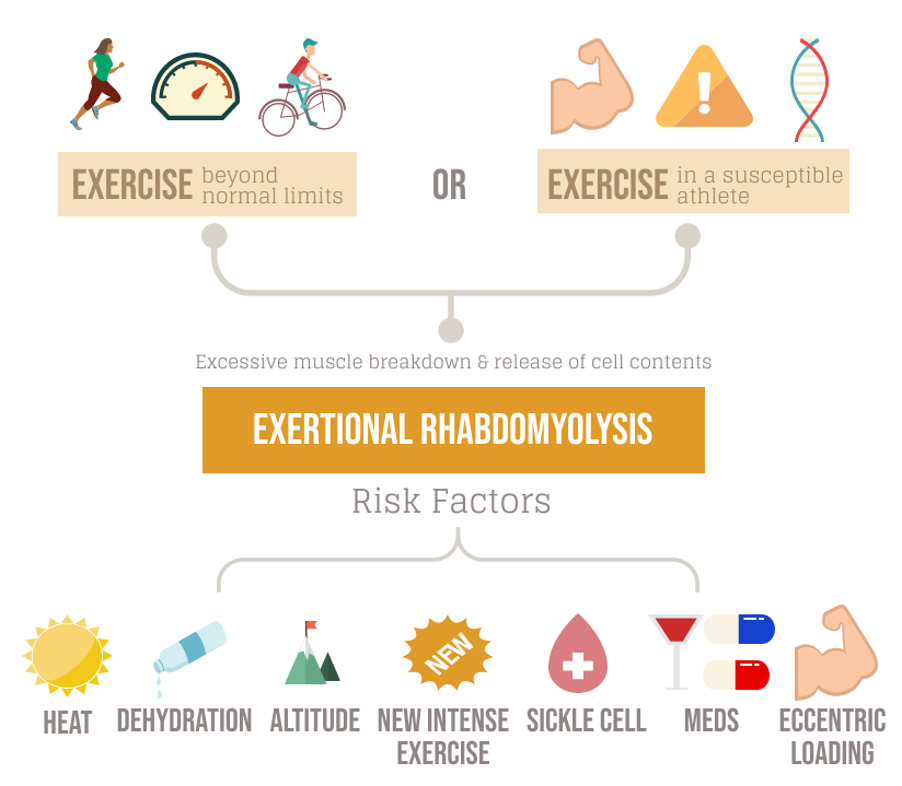
Exertional rhabdomyolysis (ER) is a condition that can impact athletes, patients and military personnel alike, causing an excessive breakdown of muscle after exercise. In some patients, this can be due to intense exercise well above the normal levels of fatigue, while those with a genetic or metabolic predisposition may experience ER through a combination of risk factors and exercise below levels of extreme fatigue. We discuss how a better understanding of the condition can lead to early diagnosis and help SEM teams reduce the risk of ER in their athletes.
There has been an increased awareness of ER in the recent past, due to its impact on athletes, particularly when exercising in extremes of heat. This condition has been shown in case series reports to affect endurance sports athletes, athletes in pre-season camps and in patients performing high volumes of eccentric circuit-based exercises (1). It is also known to potentially affect athletes at all levels of sport, including amateur, collegiate and professional sports. Currently, there is greater awareness of ER within the SEM community, either due to the incidence of the condition increasing or improved recognition and reporting.
How to diagnose Exertional Rhabdomyolysis
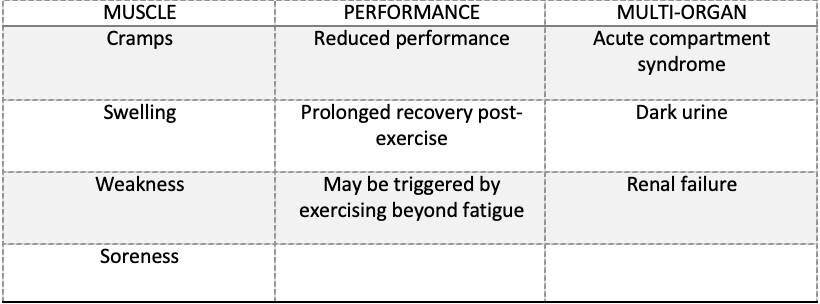
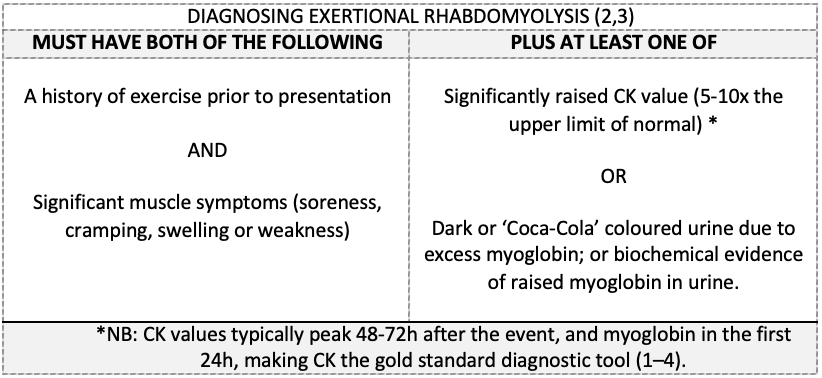
Currently, there is no consensus definition for ER, but existing criteria include a combination of clinical symptoms and evidence of muscle breakdown (creatinine kinase (CK) or myoglobin) (2,3). It has been suggested that ER may be an extreme physiological response to exercise that sits on the opposite end of the spectrum to delayed-onset muscle soreness (DOMS) (1,2).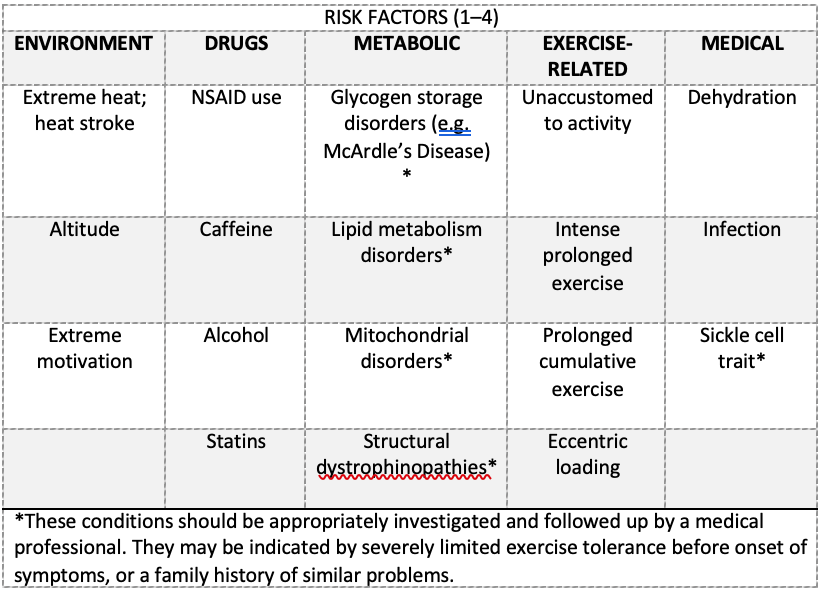
Athlete’s features
An athlete suffering from ER may expect to present with any of the following exercise-related symptoms (2–4):
The Athlete’s perspective
For many athletes, ER is an unforeseen and distressing diagnosis that results in withdrawal from training and, in some cases, hospitalisation for medical treatment. In most cases, ER is an unfortunate event due to excessive exercise in extreme conditions. However, ER may reveal an underlying (metabolic, muscle, genetic or enzyme) disorder that an athlete was previously unaware of (1). This can have a significant impact on the athlete’s long-term health, their training volumes, and they may require specialist advice to guide their recovery and subsequent return to exercise.
For patients whose occupation relies on exercising, such as elite athletes or military personnel, this can be a critical occupational concern. Protocols for a supervised return to exercise program have been published for military personnel and adapted versions are also available for elite athletes [See Table 3, Page 176, (2)].
How can SEM clinicians design exercise programs that reduce the risk of athletes developing ER?
SEM clinicians, coaches and strength and conditioning teams will have a unique insight into their athletes’ training loads. Early identification of risk factors in an athlete’s medical history, or risk assessing training and environmental conditions and monitoring for early symptoms, can help reduce the risk of ER post exercise.
The “Too-Fast Too-Soon” effect
There have been several published case reports where multiple athletes, taking part in the same intense pre-season camps have gone on to develop ER (1). “Boot-camp” style intense training blocks, in deconditioned athletes in extremes of temperature or under the effects of dehydration or drug toxicity, are associated with an increased risk of ER by increasing exercise loads “too-fast too-soon” (1).
Medical teams can reduce the risk of exposing athletes to the “too-fast too-soon” effect by incorporating hydration strategies, rest blocks and adapting training regimes for high-risk athletes. They can also monitor the use of prescribed medications or counsel athletes on the use of common over the counter anti-inflammatory medications such as NSAID’s (e.g., ibuprofen).
Prevention and follow up post Exertional Rhabdomyolysis
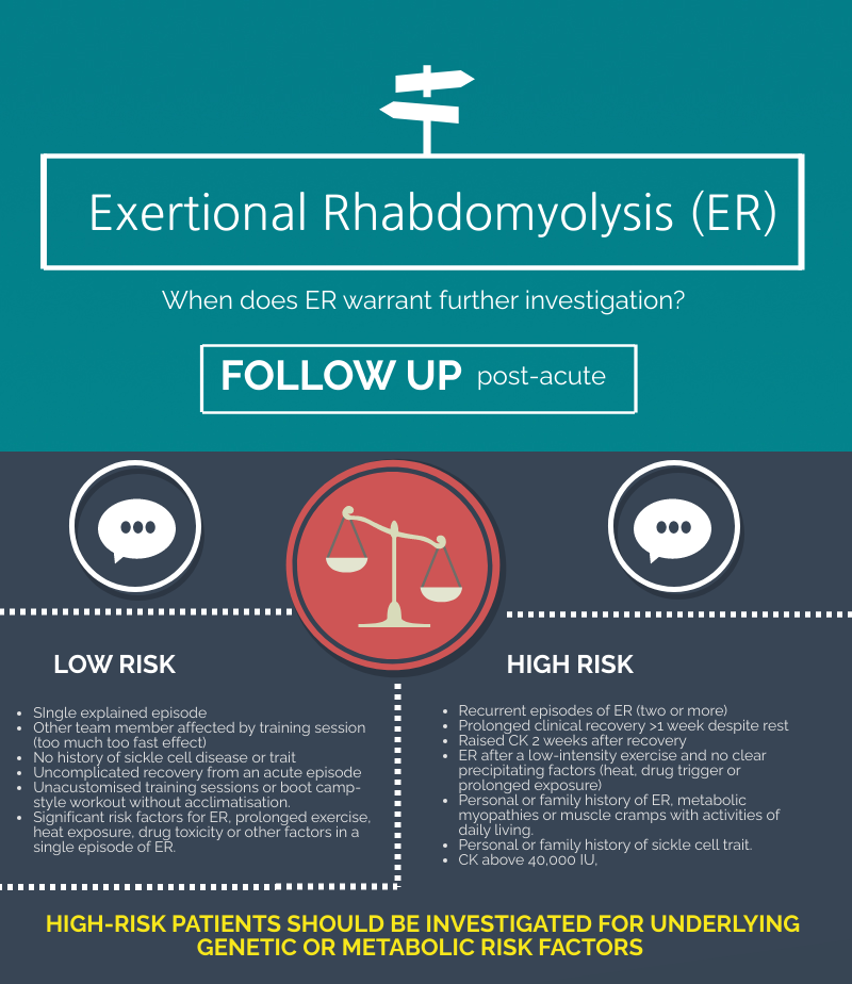
Knowledge of the key risk factors and prevention strategies amongst athletes, support staff and medical teams can reduce the risk of ER. Additional monitoring and follow-up of athletes post-ER can also help to stratify athletes into high or low-risk episodes, based on clinical history, examination and creatinine kinase response during recovery. Athletes who have had a high-risk episode should undergo appropriate investigations for any underlying medical conditions to help guide future exercise recommendations (2).
Take home points:
- ER is an extreme physiological response seen when the muscle is pushed beyond its capable limits, causing excessive muscle breakdown.
- There are discreet training, athlete and environmental risk factors that can predispose athletes to develop ER.
- These include intense, prolonged exercise, eccentric loading, genetic predispositions, deconditioned participants, heat, altitude and dehydration.
- Athletes can be split into those who are at a high and low risk of recurrence based upon a focused (SEM) exercise history.
- Knowledge of the key risk factors of ER can help athletes, support staff, and medical teams to reduce the risk of ER and help to guide athletes back to a safe return to exercise.
Author and Affiliation:
Mr Christian Pugsley, BSc (Hons SEM), is a final year UCL Medical Student, currently on elective at the ISEH, London (UK). He is interested in athlete health and performance, and the impact of exercise on the general population.
Author contact details – Twitter: @cafpugsley. Email: zchacaf@ucl.ac.uk
Artwork courtesy of: Ms Sidra Awan Senior Critical Care Pharmacist (artwork medium: charcoal and pencil)
Twitter @Rafeeki4
No conflicts of interests to declare.
References:
- Rawson ES, Clarkson PM, Tarnopolsky MA. Perspectives on Exertional Rhabdomyolysis [Internet]. Vol. 47, Sports Medicine. 2017 [cited 2021 Jun 2]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5371628/
- Nye NS, Kasper K, Marc Madsen C, Szczepanik M, Covey CJ, Oh R, et al. Clinical Practice Guidelines for Exertional Rhabdomyolysis: A Military Medicine Perspective [Internet]. 2021 [cited 2021 Jun 2]. Available from: https://journals.lww.com/acsm-csmr/Fulltext/2021/03000/Clinical_Practice_Guidelines_for_Exertional.10.aspx
- Fernandes PM, Davenport RJ. How to do it: Investigate exertional rhabdomyolysis (or not). Practical Neurology [Internet]. 2019 [cited 2021 Jun 2];19(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6580786/
- Torres PA, Helmstetter JA, Kaye AM, Kaye AD. Rhabdomyolysis: Pathogenesis, diagnosis, and treatment [Internet]. Vol. 15, Ochsner Journal. 2015 [cited 2021 Jun 2]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4365849/