By Giacomo Rossettini @GiacomoRoss86, Tommaso Geri @totomash, Alvisa Palese and Andrea Lovato
Worldwide, the Coronavirus Disease 2019 (COVID-19) is spreading. The World Health Organization (WHO) recently declared this epidemic as a Public Health Emergency of International Concern and recently a pandemic.
In Italy the number of infected people rose from 228 cases on February 24th to 110,574 cases by April 2nd–a 484% increase in 38 days. While several governmental measures have been taken (e.g., closing of schools, imposing quarantine, restricting social gatherings) [1], we as clinicians (physicians, physiotherapists, nurses) involved in sports medicine and rehabilitation asked: what role could healthcare providers play in reducing the spread of the infection? How could we help to control this unprecedented situation and limit the load on the healthcare system? Lastly, how can we can help our patients to manage this new life-threatening situation during their rehabilitation/ training sessions with us?
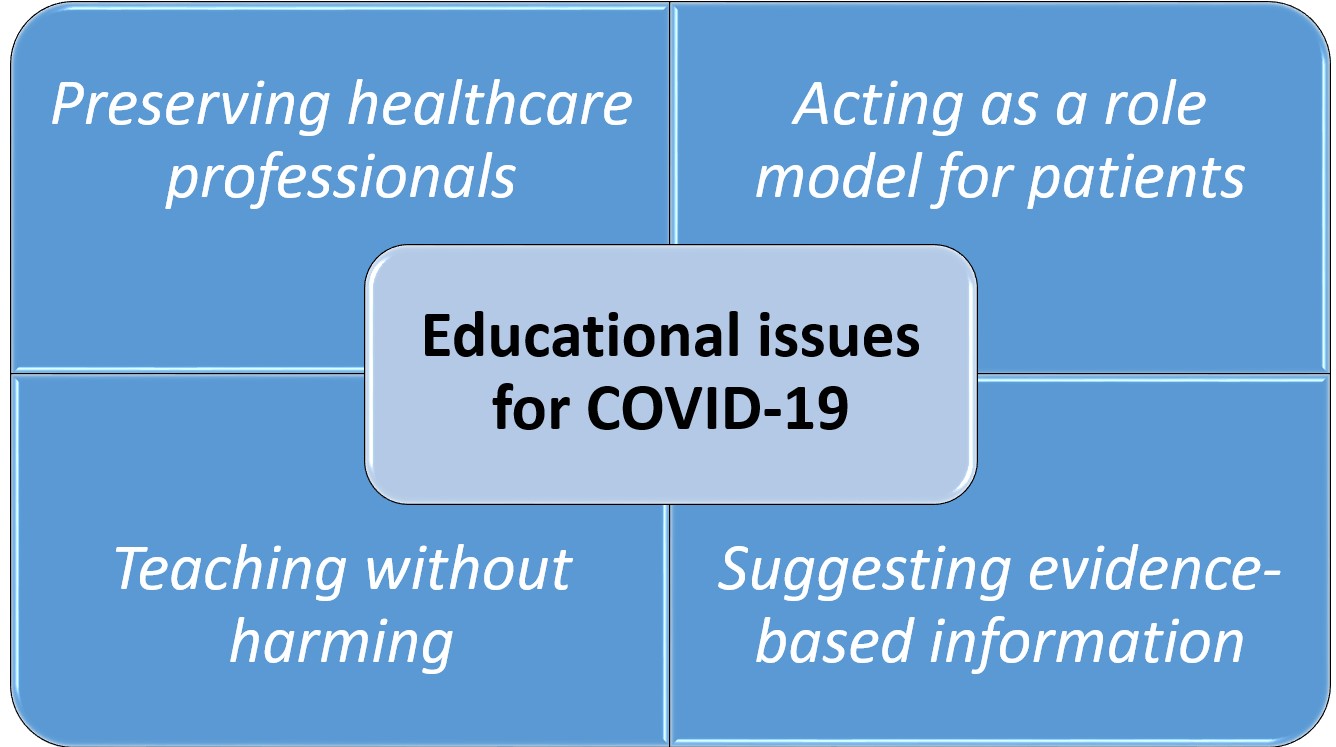
More than 100 trials are in progress to find a treatment for COVID-19 [2], and up until now we have not an effective prevention or treatment strategy- leaving other patients’ experiences as the best preventive strategy to fight it. While we are learning from our direct experience, we call to all healthcare providers to also see themselves as part of the solution. Below we highlight four educational issues that should be considered during any therapeutic interaction:
- Provide protective equipment for health professionals to continue their practice and mandate full compliance
The WHO suggests that we adopt face masks, eye protection, gloves, gowns, apron, with patients infected or suspected. It is also suggested to minimise the number of people using a room at any time during a session of rehabilitation, and to adopt hand sanitizer, soap and water, cleaning supplies. The aim with these measures are to protect healthcare providers and their patients from inhaling or having contact with aerosols and droplets that may be generated during interactions with patients.[3]
- Act as a role model and educate patients to be socially responsible
The WHO recommends that we avoid touching our eyes, nose or mouth, and frequently clean our hands with alcohol-based hand rub or soap and water. We must also clean the workplace with disinfectant regularly, and promote good respiratory hygiene (i.e., appropriately covering coughs and sneezes) so we can block any potential chains of transmission.
To protect others from getting sick, if you have a mild cough or a low-grade fever (37.5 C or more) stay home, and avoid close contact.[3]
- Teach without harming
We must educate and reassure patients, rather than catastrophizing the situation or giving pessimistic perspectives. The aim here is to limit negative psychological impacts among patients (e.g., confusion, fear, anger, anxiety, depression, stress, emotional exhaustion, stigma).[4]
- Suggest reliable and evidence-based sources of information
Effective and well-coordinated communication is a essential to control fake news, conspiracy theories and false information, particularly on social media. In this moment of crisis, it is a priority to reduce confusion among patients and the public, and have consistent clear messages to maintain trust with our audiences as health providers.[5]
It is our responsibility to coordinate efforts to reduce the spread of COVID-19, and do our best to avoid the collapse of our healthcare systems. We must involve healthcare providers when implementing recommendations provided by public health organisations, government agencies and other relevant and trusted authorities. We are confident that immediate adherence to these measures will help us tackle this unprecedented healthcare challenge.
***
Acknowledgments:
This work was developed within the framework of the DINOGMI Department of Excellence of MIUR 2018-2022 (legge 232 del 2016).
Authors
Giacomo Rossettini1, Tommaso Geri1, Alvisa Palese2 and Andrea Lovato3
1 Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genoa, Campus of Savona, Savona, Italy.
2 Department of Medical Sciences, School of Nursing, University of Udine, Udine, Italy.
3 Department of Neuroscience DNS, Audiology Unit, University of Padova, Treviso, Italy.
Corresponding author:
Giacomo Rossettini, PT, PhD.
Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genoa, Campus of Savona, Savona, Italy. Via Magliotto, 2 – 17100 Savona (SV). E-mail: giacomo.rossettini@gmail.com
Competing interests:
The Authors have nothing to declare.
References
- http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1 (data accessed on March 29th)
- Zhang T, He Y, Xu W, Ma A, Yang Y, Xu KF. Clinical trials for the treatment of Coronavirus disease 2019 (COVID-19): A rapid response to urgent need. Sci China Life Sci 2020;Published Online First: 29 February 2020. doi:10.1007/s11427-020-1660-2
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (data accessed on March 10th)
- Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020;7:228-9 doi:10.1016/S2215-0366(20)30046-8 [published Online First: 4 February 2020]
- Zarocostas, J. How to fight an infodemic. Lancet 2020;395:676 doi:10.1016/S0140-6736(20)30461-X [published Online First: 29 February 2020]