By Anna Boniface@AnnaBoniface
Low energy availability (LEA) from insufficient energy intake to fuel training demands and daily physiological processes has a negative impact to multiple systems in the body (Mountjoy et al, 2014). Adverse effects to bone health are a consequence of LEA. An athlete presenting with a bony stress injury (BSI) to a health care professional is often the precursor to Relative Energy Deficiency in Sport (RED-S). Naturally, an athlete with a significant injury will require cessation in training for bone healing. This offers a window of opportunity to correct the LEA and other health consequences that coincide.
With medical clearance and evidence of bone healing if a BSI is present, the athlete will undergo a period of rehabilitation for bone recovery. This offers a challenge for a health care professional to balance rehabilitation with energy availability. Increasing training demands whilst maintaining sufficient nutritional intake. This all depends on the athlete’s psychological readiness, and so it’s important to consider their relationship with food and exercise. A multidisciplinary team (MDT) approach is key to ensure that an athlete’s energy availability and psychological wellbeing is maintained.
Start with strength and conditioning, then aerobic training.
During the initial stages, the focus should be on strength and conditioning, and gradually introduce aerobic training. It is well established that bone responds to mechanical load it is subjected to. A combination of weight bearing aerobic training, resistance training and impact activities is ideal for bone health (Harding et al, 2017). Non-weight bearing sports such as cycling, provides no osteogenic stimulus and can have a negative impact on bone health, particularly in combination with LEA (Keay et al, 2018, 2019). Clear training parameters should be established with athletes to aid compliance to appropriate levels of training, for example training zones, duration and volume. Cardiovascular training intensity and an increase in volume should only take place in the final stages of the recovery process (Keay, 2019).
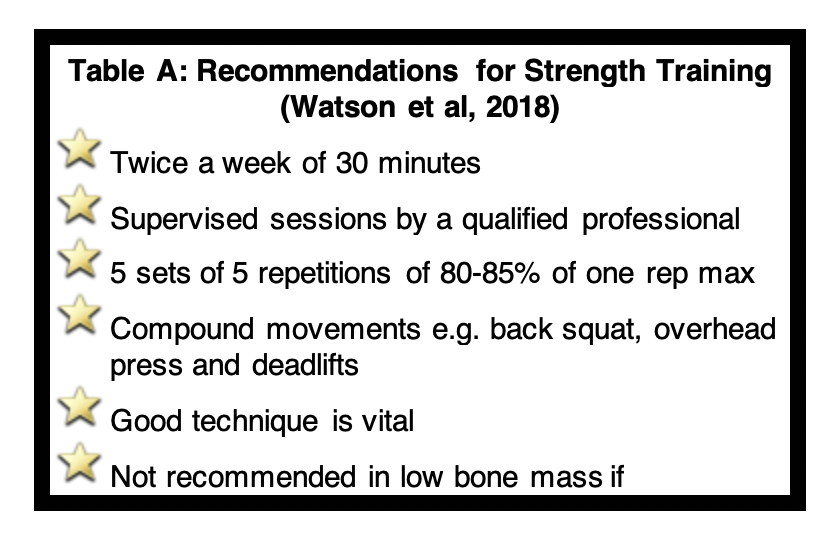
Progressive high intensity resistance training has recently been shown to have positive outcomes on bone strength (Watson et al, 2018). Recommendations in Table A suggest a supervised twice weekly strength sessions focusing on compound movements. A good technique is vital and this type of training is considered safe even in cases of post menopausal woman with low to very low bone mass (Watson et al, 2018).
Multi-directional impact on bone health
Multi-directional impact activity is known to provide the highest osteogenic stimulus to bone (Osteoporosis Australia, 2013). Prescribing impact exercises can help maintain bone health particularly in non-weight sports like cycling (Keay et al, 2018, 2019), but also when treating reduced bone mineral density (BMD) (Beck et al, 2017). When prescribing moderate to high impact weight bearing activities an individualised approach and potential risk factors should be considered by using clinical assessment tools, such as the RED-S CAT, but also considering other risk factors associated with reduced BMD e.g. steroids and smoking history. A dual energy X ray absorptiometry (DXA) scan may also be warranted to aid the prescription of impact activities. The following principles and exercise prescription is highlighted below and shown in Table B (Beck et al, 2017). With the impact loading primarily being researched in post menopausal woman, risk classification is based on T score values. Within the RED-S CAT criteria, Z score of < – 1.5 used for diagnosis of reduced bone mineral density, which is more applicable for the younger athletic/dancer population.
Click here to view: Table B- Impact Loading (Adapted from Beck et al, 2017)
Progressive impact exercises of approximately 50 contacts should be completed in sets separated by rest periods. Ideally, completing these exercises 4-7 days a week, however they should not coincide on a day the athlete is running. If the athlete is completing these exercises following a BSI, it’s important to carefully monitor their injury symptoms during and after the activity. The athlete should only progress onto the next exercise if symptom free for at least two successive sessions.
Remember to consider return to play tools available to you
It is important to ensure that an athlete is showing improvements in biomarkers, physical and mental health, but is also conditioned enough to withstand sport, particularly following a BSI. Useful return to play tools such as the The Relative Energy Deficiency in Sport Decision-based Return-to-Play Model (adapted from Creighton et al, 2010) and the RED-S Clinical Assessment Tool (Mountjoy et al, 2015) can help guide a health care professional in returning the athlete to sport. Return to running programs should be individualised and progressive according to the athlete’s response and symptoms of the injury. Table C highlights an example program adapted from Warden et al, (2014).
Click here to view: Table C – Graded Return to Run Program for Bone Stress Injury (adapted from Warden et al, 2016)
What else should you consider?
Other elements of rehabilitation that should be considered include back extension strength training, to oppose kyphotic curvature and consequently reduce vertebral fractures in the long term. In cases with spinal osteoporosis, avoiding flexion and twisting activities is encouraged (Briggs et al, 2014). Neuromuscular control and balance exercises should also be incorporated into an athlete’s rehabilitation program, to mitigate the impact of LEA on neuromuscular function (Keay, 2019).
Overall, LEA has an adverse effect to athletes’ bone health. A BSI is often the initial complaint to a health care professional prior to a RED-S diagnosis. Correcting the energy deficit and recovery following a BSI may require cessation from sport, however, exercise is an important aspect in the rehabilitation process, particularly for improvements in bone health and prevention of further BSI. Balancing an athlete’s nutritional intake, alongside rehabilitation and return to play is challenging. It requires a careful MDT approach and monitoring of key markers in RED-S recovery. Assessment tools should be used to guide a health care professional in returning an athlete to play. Key aspects of rehabilitation should include high intensity supervised resistance training, multidirectional impact activities and weight bearing aerobic exercise. Providing the athlete with clear training parameters, particularly for training intensity is vital. Only when the athlete is towards the final stages of recovery should high intensity aerobic training be introduced.
***
Anna Boniface @AnnaBoniface is a physiotherapist and marathon runner. From personal experience of RED-S and being emersed in the world of endurance sport, she is interested in the role of the physiotherapist in the rehabilitation of bone health in athletes.
References
Osteoporosis Australia 2013 – 2nd edition: https://www.osteoporosis.org.au/sites/default/files/files/Exercise%20Fact%20Sheet%202nd%20Edition.pdf
Harding, A.T, Week, B.K, Watson, S.L, Beck, B.R, 2017., The LIFTMOR-M (Lifting Intervention for Training Muscle and Osteoporosis Rehabilitation in Men) trial: protocol for a semi-randomised controlled trial of supervised targeted exercise to reduce risk of osteoporotic fracture in older men with low bone mass, British Medical Journal, 6 (7) Available online at: Accessed: 29th March 2019
Keay N, 2019. Returning to Sport/Dance restoring Energy Availability in RED-S Available at BJSM: https://blogs.bmj.com/bjsm/2019/03/26/returning-to-sport-dance-restoring-energy-availability-in-red-s/
Keay N, Francis G, Hind K., 2018. Low energy availability assessed by a sport-specific questionnaire and clinical interview indicative of bone health, endocrine profile and cycling performance in competitive male cyclists, BMJ Open Sport & Exercise Medicine, 4 (1), Available at: https://bmjopensem.bmj.com/content/4/1/e000424.infoAccessed on: 29th March 2019
Keay N, Francis G, Entwistle I, Hind K, 2019 Clinical evaluation of education relating to nutrition and skeletal loading in competitive male road cyclists at risk of relative energy deficiency in sports (RED-S): 6-month randomised controlled trial, BMJ Open Sport and Exercise Medicine, 5 (1) https://bmjopensem.bmj.com/content/5/1/e000523#DC1
Watson, S.L., Weeks., B.J., Weis, L.J., Harding., A.M., Horan, S.A., Beck, B.R, 2018. High‐Intensity Resistance and Impact Training Improves Bone Mineral Density and Physical Function in Postmenopausal Women With Osteopenia and Osteoporosis: The LIFTMOR Randomized Controlled Trial, Journal of Bone and Mineral Research 33 (2), Available at: https://onlinelibrary.wiley.com/doi/full/10.1002/jbmr.3284Accessed: 29th March 2019
Greig AM, Briggs AM, Bennell KL. 2014, Trunk muscle activity is modified in osteoporotic vertebral fracture and thoracic kyphosis with potential consequences for vertebral health. PLoS ONE 9 (10) Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0109515Accessed: 29th March 2019
Creighton DW, Shrier I, Shultz R, et al, 2010. Return-to-play in sport: a decision-based model. Clinical Journal ofSport Medicine, 20 p 379–85 Available at: https://www.ncbi.nlm.nih.gov/pubmed/20818198?dopt=AbstractAccessed: 30th March 2019
Mountjoy M, Sundgot-Borgen J, Burke L, et al. 2014. The IOC consensus statement: beyond the Female Athlete Triad—Relative Energy Deficiency in Sport (RED-S), British Journal of Sports Medicine, 48, pp 491-497, Available at: https://bjsm.bmj.com/content/48/7/491.citation-tools, Accessed on: 30th March 2019
Mountjoy M, Sundgot-Borgen J, Burke L, et al. 2015, Relative Energy Deficiency in Sport Clinical Assessment Tool, British Journal of Sports Medicine, 49: 421–423 Available at: https://bjsm.bmj.com/content/bjsports/49/7/421.full.pdfAccessed on: 30th March 2019
Warden, T.J, Davis, I.S, Fredericson, M, 2014. Management and Prevention of Bone Stress injuries in Long Distance Runners, Journal of Orthopaedic and Sports Physical Therapy, 44 (10), Available at: https://www.jospt.org/doi/pdf/10.2519/jospt.2014.5334Accessed on: 30th March 2019