This article was originally published in 2013 in the Aspetar Sports Medicine Journal and is reproduced with the kind permission of Aspetar – Orthopaedic and Sports Medicine Hospital.
Written by Daichi Hayashi, Frank W Roemer and Ali Guermazi
**Note that you can subscribe (free) to the Aspetar Sports Medicine Journal by following this link (right margin, simple!):

Handball involves running, turning and jumping which cause high levels of mechanical stress to the knee. The vigorous nature of the ball game predisposes handball players to develop osteoarthritic changes in the knee including, for example, cartilage damage, meniscal tear, ligamentous damage and bone marrow oedema-like lesions.
A recent large-scale European research study involving 15,783 athletes who had primary unilateral anterior cruciate ligament reconstruction showed male team handball players (n=1,392) had an increased risk of full-thickness cartilage damage compared to male team football (soccer) players (n=6,473)1. Another epidemiological study demonstrated playing handball was associated with symptomatic knee osteoarthritis (OA) in 295 men aged 25 to 70 seen at orthopaedic clinics2.
While knee OA is generally thought to be a major public health problem that primarily affects the elderly, handball players can have OA of the knee from a relatively younger age than persons who do not play handball or other vigorous sports that can have a similar level of mechanical stress to the knee joint. In particular, trauma-induced damage of cartilage, meniscus and ligaments can trigger acceleration of degenerative OA-related changes within the knee joint, potentially leading to the need for knee arthroplasty at a relatively young age.
The joint as an organ – not just articular cartilage!
Sports physicians should also be aware of imaging characteristics of knee OA in vigorous sports such as handball. Currently, conventional radiography is still the gold standard imaging technique for the evaluation of known or suspected knee OA in clinical practice and research. It has many important limitations that were revealed as MRI became more and more widely available3.
Traditionally, it has been thought that articular cartilage is the central feature and the primary target for evaluation and therapy. However, in reality, OA-related pathological changes may affect all structures of the knee joint. Of the commonly deployed imaging techniques, only MRI allows visual assessment of all structures of the joint, including cartilage, meniscus, ligaments, subarticular bone marrow and synovium. MRI also allows evaluation of the knee as a whole organ in a three-dimensional fashion and directly aids in the assessment of cartilage morphology and composition.
In this narrative review article, the advantages and disadvantages of conventional radiography, MRI and other techniques including ultrasound, nuclear medicine, computed tomography (CT) and CT arthrography in the imaging of knee OA are described, in the context of sports medicine and musculoskeletal radiology.
CONVENTIONAL RADIOGRAPHY
Radiography is the most readily available, least expensive and simplest imaging modality. It enables detection of OA-associated bony features such as osteophytes, subchondral sclerosis and cysts. OA is radiographically defined by the presence of marginal osteophytes3. Radiography can also determine joint space width (JSW), which is a surrogate marker of cartilage thickness and meniscal integrity4. However, precise measurement of each of these articular structures is not possible because one cannot actually visualise cartilage or meniscus on radiography unless they are abnormally calcified i.e. normal hyaline cartilage or meniscus cannot be directly evaluated using radiography. Variations in semiflexed knee positioning, which occur during image acquisition despite standardisation, can also be problematic, since such variations can affect the measurement of various radiographic parameters of OA including JSW. In the OA research field, despite these notable drawbacks, slowing of radiographically detected joint space narrowing (JSN) is the only structural end point currently recommended by the U.S. Food and Drug Administration to demonstrate efficacy of disease-modifying OA drugs in phase-III clinical trials4. Progression of JSN is the most commonly used criterion for the evaluation of structural knee OA progression, and the total loss of JSW (‘bone-on-bone’ appearance) is one of the indicators for knee arthroplasty3.
The severity of radiographic OA can be assessed semi-quantitatively or quantitatively. For semi-quantitative assessment of knee OA, the Kellgren and Lawrence (KL) grading system is a widely accepted scheme used for defining radiographic OA based on the presence of a definite osteophyte (grade 2)3. However, KL grading is limited by the fact that KL grade 3 includes all degrees of JSN, regardless of the actual severity. Alternatively, the Osteoarthritis Research Society International (OARSI) atlas uses a different approach and grades tibiofemoral JSW and osteophytes separately for each compartment (medial tibiofemoral, lateral tibiofemoral and patellofemoral) of the knee. Using either method, it should be kept in mind that centralised radiographic reading is important from the view point of observer reliability, as even expert readers seem to apply different thresholds for semiquantitative grading of JSN3.
In contrast, quantitative JSW measurements can be performed either manually or by using a semi-automated software application. JSW is the distance between the projected femoral and tibial margins on the radiographic image. Quantification of JSW using image processing software does require a digital image either digitised plain films or images acquired using fully digital modalities such as computed radiography and digital radiography. Measurements of JSW obtained from knee radiographs have been found to be reliable, especially when the study lasted longer than 2 years and when the radiographs were obtained with the knee in a standardised semiflexed position. For further details of the measurement techniques, interested readers are directed to a recent publication by Guermazi and colleagues3.
The abovementioned semiquantitative and quantitative analyses of knee radiographs are particularly relevant for clinical and epidemiological OA research. In daily clinical practice of sports physicians treating handball players, evaluation of knee joint using radiography alone is insufficient since it does not allow comprehensive assessment of the joint as a whole organ. For example, a small focal cartilage defect with intact meniscus in the same compartment may not cause JSN, and thus radiographic appearance will be normal. Moreover, assessment of menisci and ligaments are very important since those structures can potentially affect the performance of handball players. Indeed, a recent population-based study in the USA involving 710 persons aged >50 years demonstrated that MRI shows OA-related pathologies in the knee joint in most people in whom knee radiographs do not show any features of OA, regardless of pain5. Conversely, cartilage loss is not the only contributory factor to JSN but changes in the meniscus such as meniscal extrusion, subluxation or meniscal root tear can also cause JSN3. Based on these limitations of conventional radiography, there is an ongoing debate regarding of the choice of modality for imaging-based definition of OA, as well as inclusion criteria and outcome measures for knee OA clinical trials4.
MAGNETIC RESONANCE IMAGING
Because of high cost per examination, MRI is not routinely used as an initial assessment or during disease follow-up of OA patients in the general population. However, in the field of sports medicine, MRI of the knee is an essential imaging examination to be performed. MRI is a key imaging tool thanks to its ability to visualise pathologies that are not detected on radiographs i.e. articular cartilage, menisci and meniscal roots, ligaments, synovium, capsular structures and bone marrow oedema-like lesions3. All these structures are important to maintain normal function of the knee joint and high levels of performance during handball games. MRI enables the following:
- the joint can be evaluated as a whole organ,
- multiple tissue changes can be monitored simultaneously over several time points,
- pathologic changes of pre-radiographic OA can be detected at a much earlier stage of the disease,
- physiologic changes within joint tissues (e.g. cartilage and menisci) can be assessed before morphologic changes become apparent.
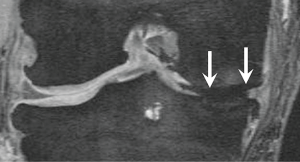
A list of knee OA features that can be evaluated using MRI are shown in Table 1. An important point to note is that one needs to select appropriate MR pulse sequences for the purpose of each study. For example, focal cartilage defects and bone marrow oedema-like lesions are best assessed using fluid-sensitive fast spin echo sequences (e.g. T2-weighted, proton density-weighted or intermediate-weighted) with fat suppression (Figure 1). 3D gradient recalled echo sequences (e.g. DESS, SPGR, FLASH) should not be used since these will underestimate the size of the lesions or may completely miss them7. Also, meniscal tears are better visualised on standard fast or turbo spin echo sequences compared to 3D gradient recalled echo sequences.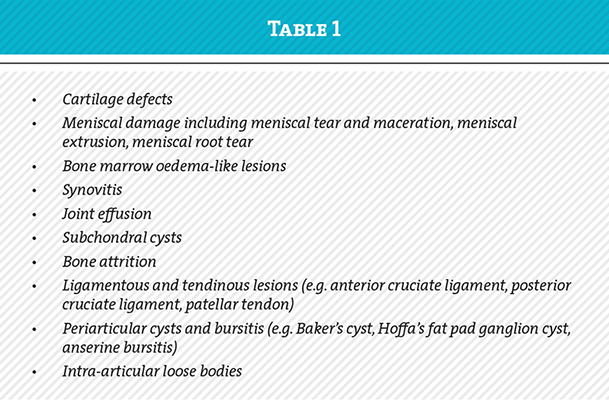
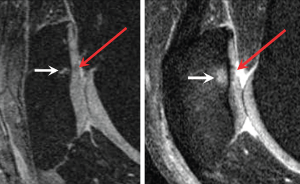
Synovitis should ideally be evaluated by using T1-weighted fat-suppressed sequences before and after intravenous administration of gadolinium to enable differentiation of inflamed synovium and effusion within the joint cavity. Both synovium and effusion show high signal intensity on non-gadolinium enhanced fluid-sensitive fast spin echo sequences and the accurate extent of synovitis cannot thus be evaluated without the use of gadolinium (Figure 2). On non-enhanced MRI, the presence of joint effusion or signal abnormalities within the Hoffa fat pad can be used as a surrogate marker of synovitis when contrast-enhanced MRI is unavailable, but these are indirect and considered less accurate than the evaluation based on contrast-enhanced MRI. Evaluation of synovitis is clinically relevant since synovitis detected by contrast-enhanced MRI is known to be associated with pain3. Another point to note is the fact that bone marrow oedema-like lesions is a non-specific finding on MRI and can represent pathologic processes that are not related to OA, such as bone contusion, spontaneous osteonecrosis of the knee and bone marrow oedema syndrome. Thus, MRI should always be interpreted in the appropriate clinical context and the interpreter needs to have knowledge of a wide range of potential differential diagnoses that bone marrow oedema-like lesions may represent. Furthermore, MRI may sometimes be affected by artifacts which degrade image quality and mimic pathological findings. For example, so-called susceptibility artifacts can be misinterpreted as cartilage damage or meniscal tear if the observer is unaware of this phenomenon.
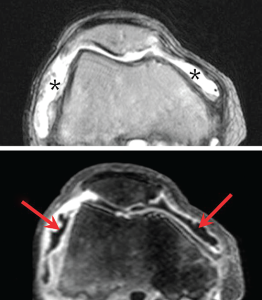
Gradient recalled echo sequences are known to be particularly prone to this type of artifact (Figure 3). In general, experienced musculoskeletal radiologists are aware of these facts and unlikely to make misinterpretations. However, it would also be beneficial for sports physicians and orthopaedic surgeons to know these important pieces of knowledge so that when they review the images themselves in reference to diagnostic reports issued by musculoskeletal radiologists they can fully understand the implications of these artifacts. To ensure optimal assessment of MRI-derived data, trained expert musculoskeletal radiologists should be consulted when designing imaging-based clinical or epidemiological OA studies and interpreting data generated in those studies.
An MRI-based definition of OA has recently been proposed for the purpose of OA research. Tibiofemoral OA on MRI is defined as either:
a) the presence of both definite osteophyte formation AND full thickness cartilage loss OR
b) the presence of one of the features in (a) AND one of the following:
- subchondral bone marrow lesion or cyst not associated with meniscal or ligamentous attachments,
- meniscal subluxation, maceration or degenerative (horizontal) tear,
- partial thickness cartilage loss and
- bone attrition6.
In addition, with MRI, OA can be classified into hypertrophic and atrophic phenotypes, according to the size of osteophytes. These newly proposed definitions and classifications are still in their infancy and are not utilised in routine clinical practice. However, given the limitations of the conventional radiography as described earlier, an MRI-based definition of OA may eventually become applicable to clinical practice in the future.
Semiquantitative and quantitative analysis of knee OA features
For research purposes, MRI features of knee OA can be evaluated using semiquantitative or quantitative approaches3. In semiquantitative assess-ment, each OA feature is graded using a defined scale (e.g. grade 0, 1, 2 and 3). A detailed review article focusing on semiquantitative MRI assessment of OA has been published recently7, and we will give an essential summary of this approach herein. There are three well-established scoring systems based on non-contrast enhanced MRI i.e. the Whole Organ Magnetic Resonance Imaging Score (WORMS), the Knee Osteoarthritis Scoring System (KOSS), and the Boston Leeds Osteoarthritis Knee Score (BLOKS), but in addition a new scoring system called the MR Imaging Osteoarthritis Knee Score (MOAKS) has been published. By integrating expert readers’ experience with all of the available scoring tools and the published data comparing different scoring systems, MOAKS was developed as a refined scoring tool for cross-sectional and longitudinal semiquantitative MR assessment of knee OA, and includes evaluation of OA features that are listed in Table 1. WORMS and BLOKS have been most widely disseminated and used, while MOAKS is new and needs more data to demonstrate its validity and reliability when applied to OA studies. For the purpose of synovitis evaluation, separate scoring systems based on contrast-enhanced MRI are available7. While WORMS, KOSS, BLOKS and MOAKS all include evaluation of synovitis using a surrogate marker, contrast-enhanced MRI-based scoring systems offer more accurate assessment because of the aforementioned reason. These scoring systems are not used in routine clinical practice and readers of this article who are not dedicated OA researchers may be unfamiliar with these, but in the field of OA research these semiquantitative scoring systems are commonly applied in both clinical and epidemiological research studies3,7. It should be noted that application and usage of these scoring systems should be done by trained expert musculoskeletal radiologists to ensure the validity and reliability of readings.
Quantitative assessment of knee OA features involves measurement of tissue dimensions such as thickness, volume, area or other numerical values. Each tissue to be analysed needs to be segmented manually or using a semi-automated or automated computer programme, and this is a labour-intensive process. For quantitative analysis of cartilage morphology, high-resolution 3D imaging sequences that delineate the bone-cartilage interface and cartilage surface with adequate contrast is required e.g. SGES and DESS sequence3. Quantitative analysis can be applied for evaluation of various knee OA pathologies, including cartilage, bone marrow oedema-like lesions, meniscus, synovitis and joint effusion, and has been used in clinical and epidemiological OA studies. However, it should be kept in mind that using segmentation approaches for ill-defined lesions such as bone marrow lesions is more challenging than segmentation of clearly delineated structures such as cartilage, menisci and effusion.
Compositional MR imaging
Compositional MR imaging allows visualisation of the biochemical properties of different joint tissues. It is therefore very sensitive to early, pre-morphologic changes that cannot be seen on conventional MRI. The vast majority of studies applying compositional MRI have focused on cartilage, although this technique can also be applied to assess other tissues including menisci and ligaments. Compositional imaging of cartilage matrix changes can be performed using advanced MRI techniques such as dGEMRIC, T1 rho and T2 mapping. For interested readers, more descriptions of these sophisticated research techniques are described elsewhere3.
Today, compositional MR imaging techniques are not used in routine clinical practice and remain sophisticated research tools that are only available at a limited number of research institutions. Nevertheless, the application in clinical trials and observational studies has been ongoing. It has been shown that composition of cartilage measured by dGEMRIC indices, T1 rho and T2 relaxation times may be related to the amount of mechanical stress to the knee joint imposed through regular exercise3. These techniques may be particularly relevant to evaluation of the knee in handball players, since a large amount of mechanical stress is regularly imposed to their knees and therefore physiological changes before morphological changes occur may be more commonly observed compared to sedentary persons in the general population. Additional novel compositional techniques include in vivo diffusion tensor imaging of cartilage based on a 7T MR system and T2* mapping of cartilage and menisci. These techniques show promise, but they will need to be practical and deployable using standard MRI systems before they can be widely used as a research or a clinical diagnostic tool.
ULTRASOUND
Ultrasound is a technique that enables multiplanar and real time imaging at a relatively low cost without radiation exposure. It has the ability to image soft tissue and to detect synovial pathology without contrast administration. Thus, it is widely used in the setting of sports medicine clinics. Limitations of ultrasound include operator-dependency and the fact that physical properties of sound limit its application to assess deeper articular structures and the subchondral bone.
In inflammatory arthritis ultrasound is more sensitive than radiography in detecting cortical lesions (erosions) and has reasonable sensitivity compared to MRI. There is no reason to believe the ability to detect cortical bone pathology should differ in OA. In contrast, subchondral bone changes (e.g. bone marrow oedema-like lesions) are not readily demonstrable by ultrasound, because the interface between soft tissue and bony cortex is highly reflective, preventing sound waves from penetrating the cortex and hence preventing visualisation of pathology deep to the cortex.
Cartilage is easily identified and ultrasound is sensitive to physical properties of cartilage. However in actual clinical practice, non-invasively visualising the cartilage in central load-bearing areas of a joint is difficult in vivo, and the clinical relevance of visible articular cartilage is questionable.
The ability to detect synovial pathology is perhaps the major advantage ultrasound has over radiography. Ultrasound-detected grey scale synovitis has been validated against arthroscopy, MRI and histology in large joint OA and ultrasound appears to be more sensitive than clinical examination in detecting synovial hypertrophy and effusions. Additionally, Doppler signal is an indirect measure of increased synovial vascularity in large joint OA. Ultrasound-detected inflammatory features seem to be correlated with knee pain in motion in patients with knee OA. Ultrasound has also been used to assess clinical response to steroid injection but further research studies are needed to demonstrate the utility of ultrasound for this purpose3.
COMPUTED TOMOGRAPHY
CT is a valuable tool for the characterisation of OA especially when imaging of osseous changes or detailed pre-surgical planning is required for knee arthroplasty. Development of helical multidetector CT systems enabled acquisition of isotropic voxels and multiplanar reconstructions in any given plane with equal quality to the original plane. Depiction of cortical bone and soft tissue calcifications by CT is superior to that by MRI. A high sensitivity was shown for CT in detection of intra-articular loose bony fragments in peripheral joints. Drawbacks of CT are low soft tissue contrast and relatively high dose of ionising radiation3.
CT AND MR ARTHROGRAPHY
CT or MR arthrography enables assessment of articular cartilage with a high anatomical resolution in multiplanar fashion. CT arthrography can be performed using a single (iodine alone) or double-contrast (iodine and air) technique. To avoid beam-hardening artifacts, the contrast material can be diluted with saline or local anaesthetics. For MR arthrography, gadolinium-DTPA is injected intra-articularly to visualise superficial cartilage defects. These arthrographic examinations have a low risk of infection from the intra-articular injection. Other potential risks include pain and vasovagal reactions, and systemic allergic reactions. CT arthrography exposes patients to radiation but MR arthrography does not.
Currently, CT arthrography is considered to be the most accurate method for assessing articular cartilage surface damage. It offers high spatial resolution and high contrast between the low attenuating cartilage and high attenuating superficial (contrast material filling the joint space) and deep (subchondral bone) boundaries. Meniscal tear can also be visualised due to the presence of contrast within the tear. CT arthrography is also ideally suited to depict subchondral bone sclerosis and osteophytes. As for subchondral changes, MR arthrography, but not CT arthrography, allows delineation of bone marrow oedema-like lesions on the fluid-sensitive sequences with fat suppression. Both techniques enable visualisation of central osteophytes, which are associated with more severe changes of OA than marginal osteophytes.
NUCLEAR MEDICINE
Scintigraphy utilises radiopharmaceu-ticals to visualise skeletal metabolism, to contribute to the localisation of disease and to assess severity of pathologic changes in OA. 99mTc- hydroxymethane diphosphonate scintigraphy shows increased activity during the bone phase in the subchondral region and is thought to reflect osteoblastic activity of early cartilage loss. While scintigraphy has excellent sensitivity, is relatively inexpensive and is readily available, limitations of the technique for the assessment of OA include its poor specificity and radiation exposure.
Positron emission tomography (PET) demonstrates metabolic changes in target tissues and can detect foci of inflammation, infection and tumours. PET utilises 2-18F-fluoro-2-deoxy-D-glucose (FDG) and reflects glucose metabolism in different tissues. Increased FDG uptake in areas of subchondral bone marrow corresponding to MRI-detected bone marrow oedema-like lesions may be seen. However, the value of FDG-PET for the assessment of OA in a clinical and research setting remains to be shown. Limitations of this modality are its limited availability, radiation and costs.
RELEVANCE OF OA IMAGING RESEARCH TO CLINICAL PRACTICE IN SPORTS MEDICINE
With many current ongoing research efforts for imaging evaluation of knee OA, more advanced imaging techniques such as compositional MRI for evaluation of physiologic changes in cartilage and menisci may eventually find their role in clinical management of patients with knee OA in athletes. Currently, without any effective disease modifying drugs being available, radiographic evaluation is considered sufficient for managing most patients and CT is used for preoperative planning before knee arthroplasty. MRI is implemented mainly for reasons of differential diagnosis and to evaluate for concomitant muscular, ligamentous or other soft tissue pathologies as well as to rule out complications of disease. As MRI findings may not necessarily translate into clinical symptoms, interpretation of these images always needs to be done in the appropriate clinical context for each patient5. When preventive strategies become more widely implemented it is to be expected that potentially more advanced techniques such as compositional MRI will find their way into clinical practice.
SUMMARY
Radiography is the initial imaging examination to be performed for the assessment of knee OA. However, in the context of sports medicine MRI is the most important imaging tool for accurate and detailed assessment of the knee joint as a whole organ. CT and MR arthrography are also useful for detailed assessment of cartilage surface damages. Sports physicians need to be aware that the choice of appropriate MR pulse sequence for the purpose of each type of pathological feature is essential for accurate and valid evaluation. Experienced musculoskeletal radiologists should be consulted to avoid potential misinterpretation of artifacts as pathological findings.
Daichi Hayashi M.D., Ph.D.1,2
Frank W Roemer M.D.1,3,4
Ali Guermazi M.D., Ph.D.1
1. Quantitative Imaging Center (QIC), Boston University School of Medicine, Boston, USA and Aspetar Orthopaedic and Sports Medicine Hospital, Doha, Qatar.
2. Bridgeport Hospital, Yale University School of Medicine, Bridgeport, USA
3. University of Erlangen-Nuremberg, Erlangen, Germany
4. Klinikum Augsburg, Augsburg, Germany
Contact: guermazi@bu.edu
References
- Røtterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Årøen A. Effect of gender and sports on the risk of full-thickness articular cartilage lesions in anterior cruciate ligament-injured knees: a nationwide cohort study from Sweden and Norway of 15 783 patients. Am J Sports Med 2011; 39:1387-1394.
- Vrezas I, Elsner G, Bolm-Audorff U, Abolmaali N, Seidler A. Case-control study of knee osteoarthritis and lifestyle factors considering their interaction with physical workload. Int Arch Occup Environ Health 2010; 83:291-300.
- Guermazi A, Hayashi D, Roemer FW, Felson DT. Osteoarthritis: a review of strengths and weaknesses of different imaging options. Rheum Dis Clin North Am 2013; 39:567-591.
- Guermazi A, Roemer FW, Felson DT, Brandt KD. Motion for debate: osteoarthritis clinical trials have not identified efficacious therapies because traditional imaging outcome measures are inadequate. Arthritis Rheum 2013; 65:2748-2758.
- Guermazi A, Niu J, Hayashi D, Roemer FW, Englund M, Neogi T et al. Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study). BMJ. 2012; 345:e5339.
- Hunter DJ, Arden N, Conoghan PG, Eckstein F, Gold G, Grainger A et al. Definition of osteoarthritis on MRI: results of a Delphi exercise. Osteoarthritis Cartilage 2011; 19:963-639.
- Guermazi A, Roemer FW, Haugen IK, Crema MD, Hayashi D.MRI-based semiquantative scoring of joint pathology in osteoarthritis.Nat Rev Rheumatol. 2013; 9:236-251.