Will you be providing first-aid care to athletes in a non-elite setting?

This guidance (in pdf format at the end of the document) defines and rationalises emergency and first aid care during the current time of heightened awareness of contracting and transmitting COVID-19. This follows on from an elite sport framework which uses Public Health England (PHE) policy and the UK Government guidance on return to sport and recreation[1],[2]. Please refer to any regional variation as applicable to your area of practice. We attempt to address the potential consequences of returning to sport, whilst balancing the risk of exposure to both the participant and the medical responder. At all times social (physical) distancing in addition to strict personal and environmental hygiene measures, are paramount in reducing infection rates and transmission of COVID-19. It must be acknowledged that any standard operating procedures (SOP) put into place on return to training can only act as a risk mitigation measure for COVID-19 transmission; a zero risk environment cannot be achieved.
Practitioners should remain up to date with Public Health and government authority guidance on COVID-19 case management, and Personal Protective Equipment (PPE) recommendations. Any update of Resuscitation Council UK (RCUK), Public Health England (PHE) guidance, or updated guidance from the equivalent body in other countries supersedes the content of this document.
General Rationale
COVID-19 is the infection caused by the Novel Coronavirus SARS-CoV-2. Respiratory droplets containing virus particles can be produced from coughing, sneezing, and forceful breathing and form the main route of transmission, either via contact with contaminated surfaces or airborne transmission following aerosolisation of respiratory secretions.[3]
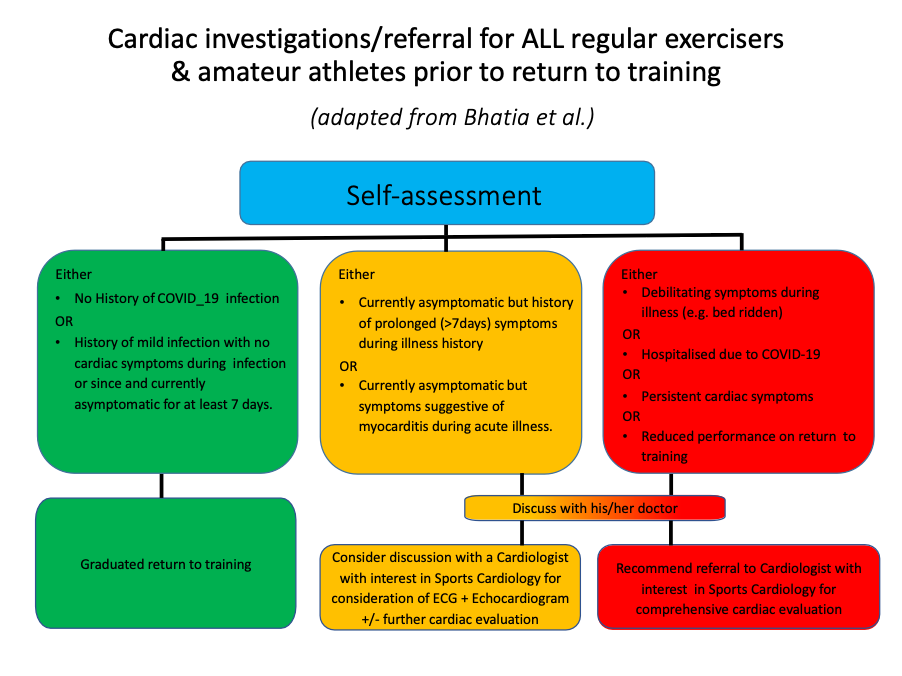
Although the COVID-19 infection is relatively novel, adverse cardiac and respiratory outcomes, with potentially serious acute and long-term sequelae, have been acknowledged in a significant proportion of affected individuals irrespective of illness severity.[4] Up to 30% of hospitalised COVID-19 patients demonstrate elevated Troponin levels indicative of myocardial injury with multiple plausible explanations, including myocardial necrosis due to myocarditis. Consequently, there are justifiable concerns that exercise in the context of an acute or recent COVID-19 infection may pose a risk for malignant arrhythmias and in extreme cases sudden cardiac death.[5] In an attempt to mitigate the risk of exercise-induced complications due to myocardial injury from COVID-19, scientific bodies recommend screening of athletes with specialist review and investigations where medically indicated prior to return to training, paired with a graduated return to play protocol.4
Most recommendations are investigation intense as they are aimed for the higher echelons of sport and financially endowed organisations. It is recognised that the level of medical provision/first aid below the elite level varies across different governing bodies, sporting levels, settings and countries. This framework seeks to provide structure for those circumstances where health care professionals are provided (Tier 1) and where emergency care is provided by first aid responders (Tier 2).
Priorities for Organisations that manage Non-Elite Sport in the context of Emergency/First Aid Care
- Conduct an emergency and first aid risk assessment and amend Emergency Action Plans (EAPs) to mitigate identified risks. Include modifications to the emergency/first aid kit, provision of personal protective equipment (PPE) and plans should individuals present with symptoms whilst at training
- All Health Care Professionals (HCPs) and first aid responders should be aware of all EAPs before entering the environment for the first time.
- Attempts should be made to identify Individuals involved in the sporting environment considered to be at a higher risk of severe COVID-19 infections[6] and mitigation strategies applied as appropriate.
- Para-sport athletes and those participants with underlying health conditions are recommended to undertake a pre participation check with a healthcare professional, to determine their own personal risk, health and vulnerability
- Optimal personal and environmental hygiene should be practised at all times by all individuals within the sporting environment (see Table 1).
- Adherence to government social/physical distancing restrictions (preferably 2m) at all times[7] except in times of delivery of emergency care where appropriate PPE is provided
- Consideration of self-screening for participants (see Table 2) as a means of minimising those with COVID-19 or suspected COVID-19 of attending a training session or competition and therefore minimising transmission.
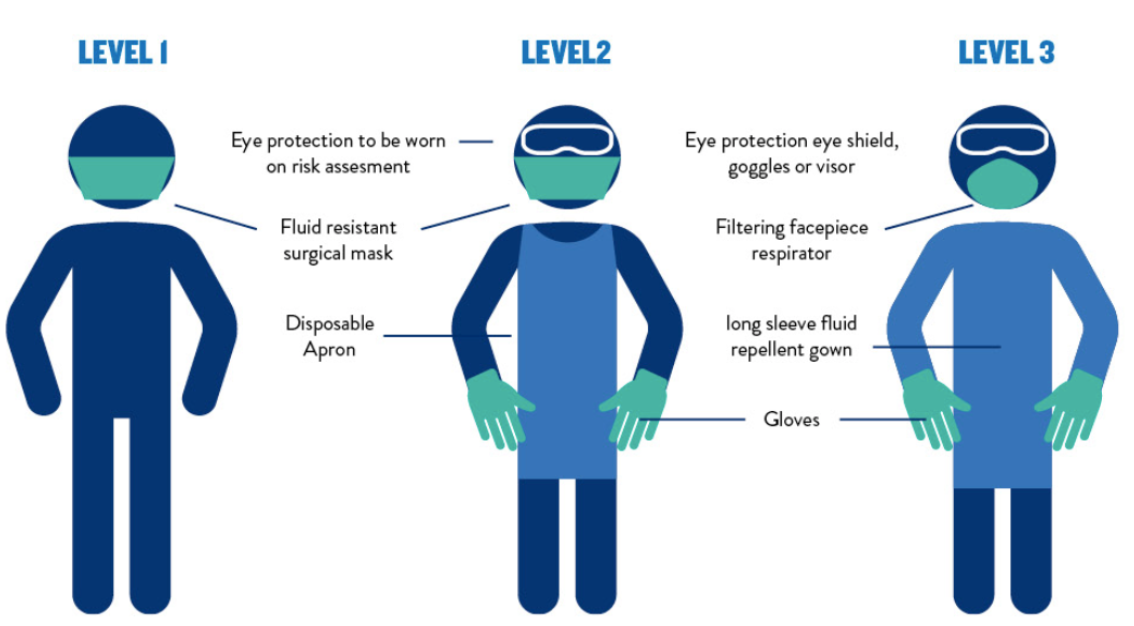
- Where HCPs and first aiders are provided, ensure the appropriate type and quantity ofPPE[8] are available at all times (see Table 3/Figure 1) and that appropriate training (including donning and doffing)[9],[10] is accessible. PPE must reflect all potential medical and first aid situations that may arise through the course of related sporting activity. Please refer to table 2 regarding single use, sessional use and reusable PPE guidance[11]
- Implementation of systematic cleaning protocols with the appropriate cleaning products and techniques, for environments and equipment; both first aid and sporting[12],[13]. Where this is not practical, clean duplicate equipment should be made available.
- Correct discarding of all PPE and contaminated equipment as per the country/local authorities’ clinical waste policy[14] , which will require a clinical waste bin and appropriate disposal procedure.
Table 1: Practices to keep everyone safe
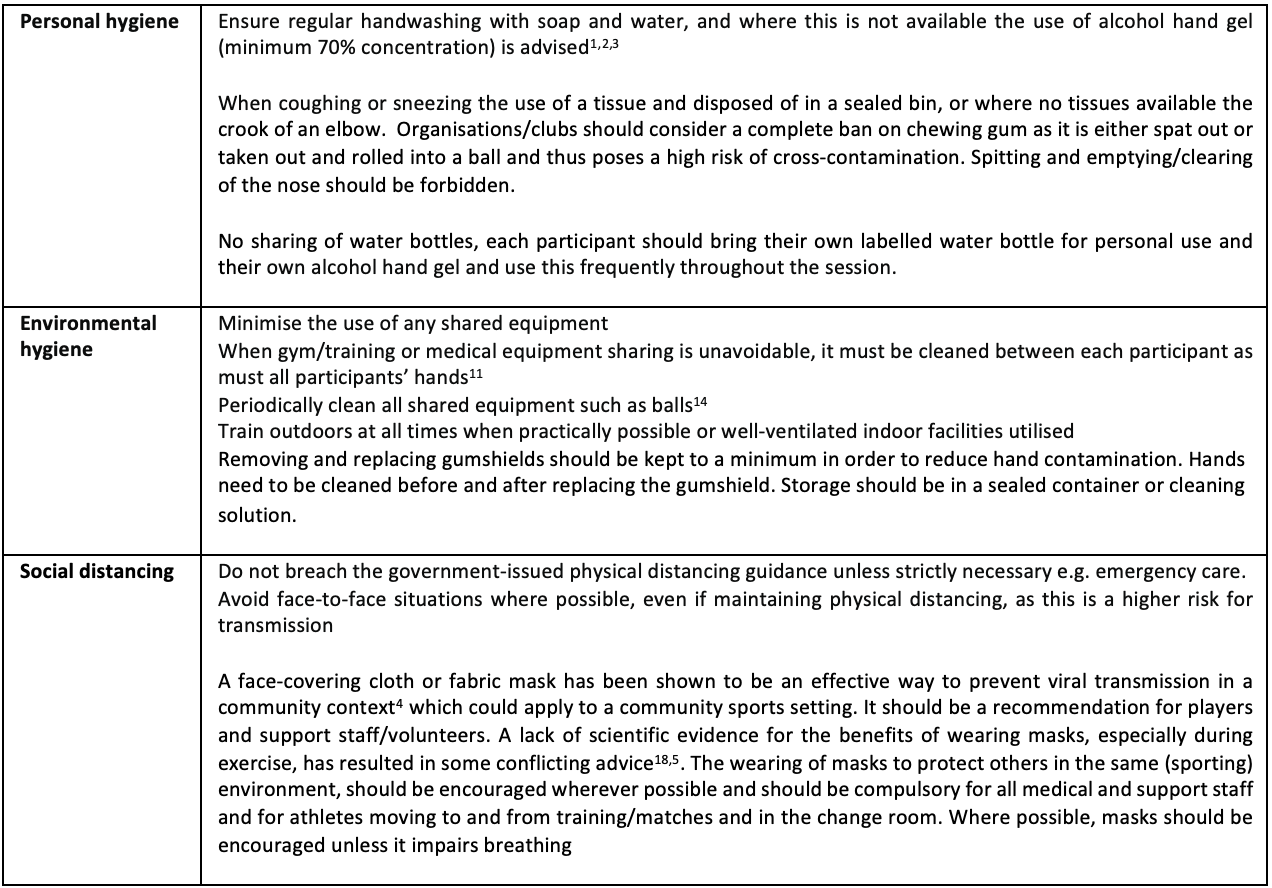
Table 2: Example of a self-screening check list prior to each training session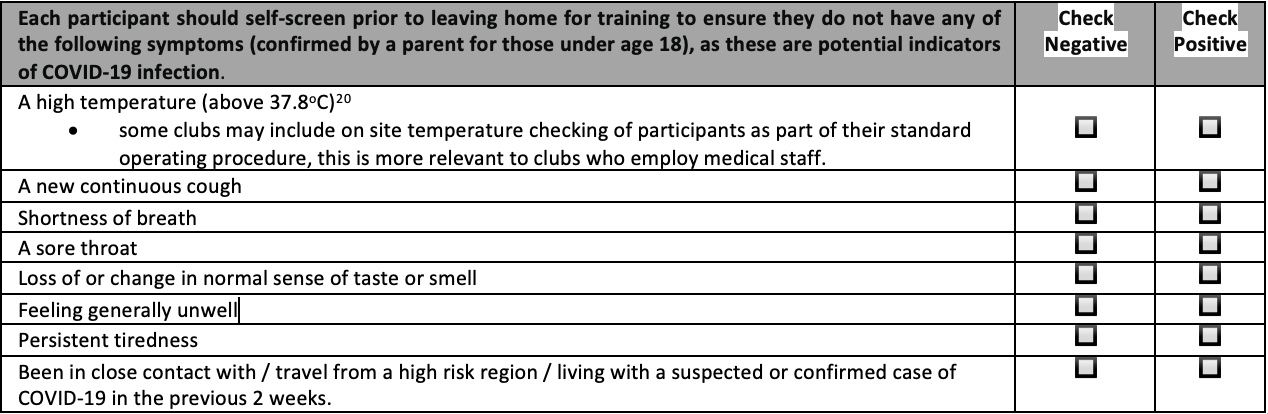
The rest of the document relates to other critical issues that first-aiders will no doubt be eager to learn more about – the practicalities of isolation, PPE, aerosol generating procedures and return-to-sport guidelines. To read more about these than what is provided in the images below, follow the link here to the pdf. Emergency and first aid care- a framework for organised non-elite sport during the COVID-19 pandemic
PDF: Emergency and first aid care- a framework for organised non-elite sport during the COVID-19 pandemic
Authors
Lisa Hodgson. Gemma Phillips. Sanjay Sharma. Michael Papdakis. Clint Redhead. Charlotte Cowie. Andy Massey. Richard Weiler. Prabhat Mathema. Jo Larkin. Jonathan Gordon. John MacLean. Mike Rossiter. Richard Tingay. Niall Elliott. Jonathan Hanson. Simon Spencer. Rod Jaques. Jon S Patricos
References
[1] Appendix I – Hand washing
[2] Appendix II – Rub washing
[3] https://www.resus.org.uk/covid-19-resources/statements-covid-19-hospital-settings/resuscitation-council-uk-statement-covid-1
[4] https://blogs.bmj.com/bjsm/2020/06/12/should-people-wear-a-face-mask-during-exercise-what-should-clinicians-advise/
[5] https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters
[6] https://www.gov.uk/government/publications/covid-19-guidance-for-ambulance-trusts/covid-19-guidance-for-ambulance-trusts
[1] https://www.gov.uk/government/publications/coronavirus-covid-19-guidance-on-phased-return-of-sport-and-recreation
[2] https://blogs.bmj.com/bjsm/2020/07/08/pitch-side-emergency-care-personal-protective-equipment/
[3] https://apps.who.int/iris/bitstream/handle/10665/331695/WHO-2019-nCov-IPC_PPE_use-2020.3-eng.pdf
[4] Bhatia R et al, Eur J Prev Cardiol 2020
[5] https://jamanetwork.com/journals/jamacardiology/fullarticle/2766124
[6] https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html
[7] https://www.gov.uk/government/publications/staying-alert-and-safe-social-distancing/staying-alert-and-safe-social-distancing
[8] https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe
[9] https://www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-non-aerosol-generating-procedures
[10] https://www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-aerosol-generating-procedures
[11] https://www.gov.uk/government/publications/covid-19-decontamination-in-non-healthcare-settings/covid-19-decontamination-in-non-healthcare-settings
[12]https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/877533/Routine_decontamination_of_reusable_noninvasive_equipment.pdf
[13] https://www.who.int/publications/i/item/cleaning-and-disinfection-of-environmental-surfaces-inthe-context-of-covid-19
[14] https://www.hse.gov.uk/healthservices/healthcare-waste.htm
[15] Appendix I – Hand washing
[16] Appendix II – Rub washing
[17] https://www.resus.org.uk/covid-19-resources/statements-covid-19-hospital-settings/resuscitation-council-uk-statement-covid-1