It’s common knowledge that being physically active is better than sitting on the couch. Numerous studies have demonstrated the abundant benefits of physical activity.1,2 Luckily, one does not have to become an athlete to profit from these advantages, because even moderate levels of physical activity are sufficient to lower the risks.3 Despite overwhelming evidence on the importance of exercise in the prevention and treatment of non-communicable diseases (NCDs), exercise programmes are poorly translated into practice.
An example of a highly prevalent NCD is peripheral artery disease (PAD), which affects more than 200 million adults worldwide, and about 850,000 in the UK. The most common symptomatic manifestation is intermittent claudication (IC), a cramping leg pain that develops during walking and is relieved with rest. Direct consequences of IC are walking impairment and reduced quality of life. Additionally, it is associated with a significantly increased risk of cardiovascular events, morbidity and mortality.
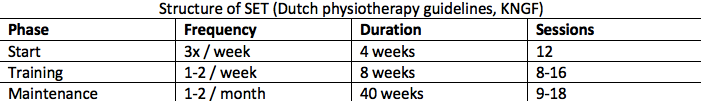
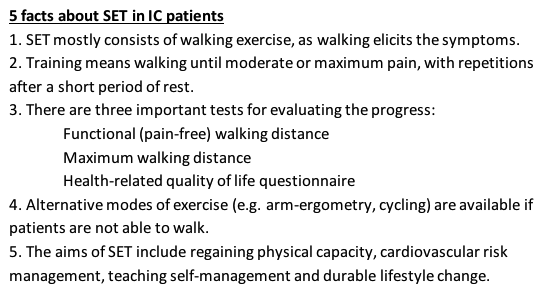
Currently, all PAD guidelines recommend supervised exercise therapy (SET) as primary treatment in IC patients.4-6 SET typically consists of walking exercise for a minimum of two hours per week for at least three months, and patients are expected to train at home as well. Invasive treatment should be reserved for patients in which SET is not successful. In support of the efficacy of exercise, two recent meta-analyses of randomised controlled trials report that SET is as effective as endovascular revascularisation in improving walking distance and quality of life.7,8 Thus, invasive and expensive interventions offer no superior functional outcomes compared to exercise rehabilitation.
Despite clear evidence, exercise rehabilitation programmes for PAD are vastly underused due to organisational barriers, such as suboptimal referral, limited accessibility, and reimbursement issues. Moreover, a patient’s lack of motivation can be a serious issue as it requires a certain effort to adhere to the SET programme. In this perspective, a ‘quick fix’ (i.e. invasive treatment) might still sound attractive for the poorly informed. This unjust preference is reinforced by the fact that in most western countries invasive treatment is reimbursed in contrast to SET.
To overcome these barriers, we established a nationwide community-based physiotherapy network (ClaudicatioNet) in 2011 to effectuate the exercise prescription for IC in the Netherlands.9 Currently, 15,000 patients with claudication per year are treated within this network by almost 2000 specialised physiotherapists. To facilitate referral, vascular surgeons and primary care physicians use our digital referral system to find the nearest affiliated physiotherapist, who will invite the patient for their first appointment. The results of treatment and disease specific outcomes are monitored via a digital quality system. This creates transparency, and quality is warranted by sharing knowledge within the network and internationally through scientific publications.
ClaudicatioNet physiotherapists are not only specialised in improving walking distance and physical activity, but also address other lifestyle factors, such as smoking, basic nutritional matters and medication compliance. Motivating patients to change behavior can be a difficult and frustrating challenge. To assist patients to adopt and sustain healthy behavior, ClaudicatioNet physiotherapists are required to complete courses in motivational interviewing and lifestyle management. We also acknowledge the importance of psychological risk factors, such as stress, pessimism, anxiety, and depression, which are common among NCD patients and promote negative health behaviour and increase cardiovascular risk.10 Therefore, we are currently implementing emotional health as an essential part of the healthy lifestyle action plan.
The stepped care approach for IC proved to be successful and highly cost-effective with savings up to 34M euro’s a year for IC treatment alone. Since January 2017, SET is fully covered for all patients by the basic health insurance in the Netherlands. We believe that a community-based physiotherapy network, with a combination of exercise therapy and lifestyle management, could also be beneficial for other NCDs. Especially since the risk factors and rehabilitation programmes for PAD, ischemic heart disease, chronic obstructive pulmonary disease, and diabetes mellitus largely overlap.11-13 Unfortunately, the implementation barriers are also comparable to those seen in PAD. Given the success of ClaudicatioNet, this approach could be used as a blueprint to tackle the challenge of translating exercise guidelines for NCDs into clinical practice.
We are interested in your responses. What do you think of the idea of community-based physiotherapy networks to translate what guidelines already advice into practice? And in what way could efforts be joined to tackle this challenge on a global level? Email Sandra your thoughts: sandra.jansen@catharinaziekenhuis.nl

SCP Jansen (MD) PhD-student at the CAPHRI Research School Maastricht and the vascular surgery department of the Catharina Hospital Eindhoven. No competing interests.
EV Rouwet (MD, PhD) Vascular surgeon at the Erasmus Medical Centre, Rotterdam. No competing interests.
JAW Teijink (Prof, MD, PhD) Vascular surgeon at the Catharina Hospital Eindhoven, professor of Integrated Care in Vascular Disease at CAPHRI Research School Maastricht, co-founder and chairman of ClaudicatioNet. Twitter: @joepteijink
References
- Kujala UM. Evidence on the effects of exercise therapy in the treatment of chronic disease. Br J Sports Med. 2009;43(8):550-555
- Pedersen BK, Saltin B. Exercise as medicine – evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25 Suppl 3:1-72.
- ‘The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 countries: the PURE study’ – What it all means December 15, 2017; The Physical Activity and Population Health BJSM Blog Series
- NICE Guideline Development Group. Peripheral arterial disease: diagnosis and management. National Institute for Health and Care Excellence (Internet). Published 2012. Last updated February 2018. Available from: https://www.nice.org.uk/guidance/cg147/chapter/Recommendations
- Gerhard-Herman MD, Gornik HL, Barrett C, et al. 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. 2017;135(12):e686-e725.
- Authors/Task Force M, Aboyans V, Ricco JB, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg.
- Pandey A, Banerjee S, Ngo C1, et al. Comparative Efficacy of Endovascular Revascularization Versus Supervised Exercise Training in Patients With Intermittent Claudication: Meta-Analysis of Randomized Controlled Trials. JACC Cardiovasc Interv. 2017 Apr 10;10(7):712-724. doi: 10.1016/j.jcin.2017.01.027.
- Fakhry F, Fokkenrood HJ, Spronk S, Teijink JA, Rouwet EV, Hunink MGM. Endovascular revascularisation versus conservative management for intermittent claudication. Cochrane Database Syst Rev. 2018 Mar 8;3:CD010512. doi: 10.1002/14651858.CD010512.pub2.
- Hageman D, van den Houten MM, Spruijt S, et al. Supervised exercise therapy: it does work, but how to set up a program? J Cardiovasc Surg (Torino). 2017 Apr;58(2):305-312. doi: 10.23736/S0021-9509.16.09825-6.
- Rozanski A. Behavioral cardiology: current advances and future directions. J Am Coll Cardiol. 2014;64(1):100-110.
- Smith SC, Jr., Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58(23):2432-2446.
- Colberg SR, Sigal RJ, Yardley JE, et al. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065-2079.
- American Association of Cardiovascular and Pulmonary Rehabilitation Guidelines for Pulmonary Rehabilitation Programs. Human Kinetics. 4 ed.2011.