Culture is notoriously difficult to define because it is made up of so many components and influenced by so many factors. One characterisation of culture is that it is the ‘distinctive norms, beliefs, principles and ways of working that combine to give each organization its distinct character’ (1). West et al. argue that the priorities leaders focus on and what they reward has a great influence on shaping organizational culture (2). Culture is also shaped by ‘formal organizational values’ (3).
NHS organizations have traditionally sought to nurture positive cultures by adopting a series of branded values, which are usually emblazoned on all organizational literature and media. These sentiments are echoed by Dr Abdul Zubairu, who argues in a previous BMJ Leader blog (4) that ‘organisational values form the basis and foundation of any organisation’, to explain why he helped create the values for his GP Federation (4). Dr Zubairu goes on to explain the challenges of embedding branded values (e.g. a lack of buy-in) and explains steps to instil values in practice (4).
However, Waheed et al. (5) have an opposing view to the prevailing perception of branded organisational values. In their BMJ Leader study (5), (in which they ‘obtained Organisational values for 221 of 228 NHS trusts, with 985 values in total’) they explored the impact of branded/individualised organisational values on key performance indicators, such as sickness absence rates, CQC ratings and NHS Staff Survey Responses. Waheed et al. conclude that “A trust’s adoption of individualised organisational values does not seem to make a positive difference to its patients or staff”, and exhort organisations to exercise caution in seeking to implement “value-defining initiatives” that have no measurable benefits (5).
Branded organisational values are often regarded as the starting point when there is talk of culture change. However, these more likely represent inputs to culture which may have very little to do with negative outputs that have a different underlying pathology. (This characterisation of culture is depicted in Diagram 1).
Diagram 1. Inputs and outputs of culture.
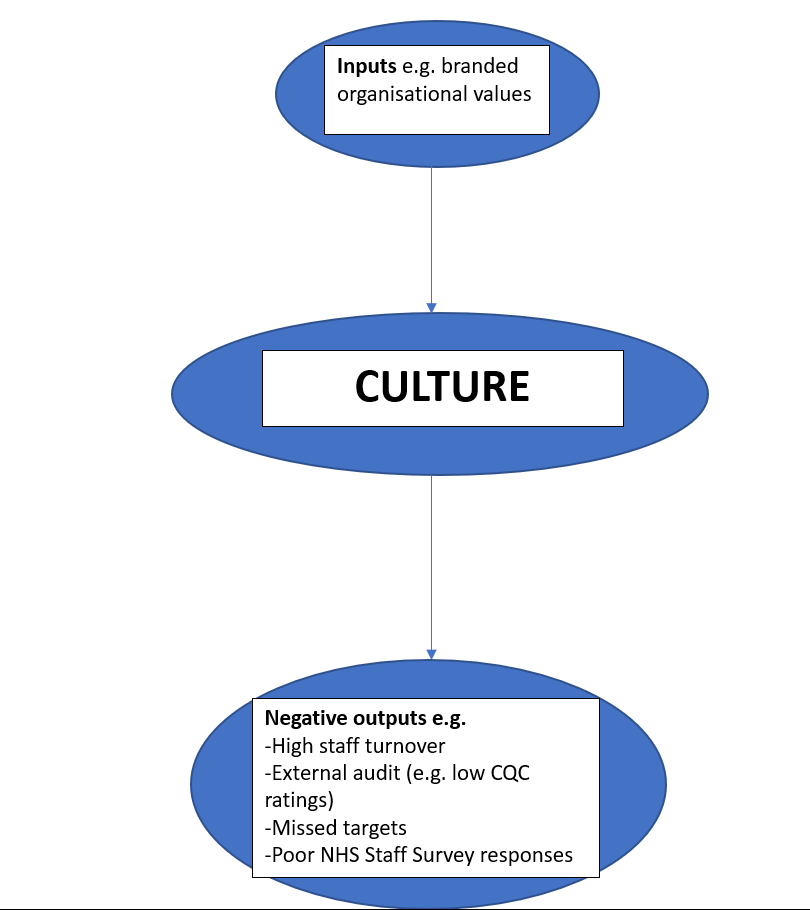
Instead of relying on a series of branded values, I believe organisations should be on the look-out for different red flags (i.e. negative outputs) or ‘signs and symptoms’, which are indicative of underlying problems in the organisation’s culture.
This characterisation of organisational culture fits the profile of a disease-model. In a disease-model, a series of risk factors give rise to a disease, manifested by its own signs and symptoms, that has a unique diagnosis and treatment regimen (6).
A representation of this for a cultural “sign and symptom” is highlighted in Diagram 2.
Diagram 2. Disease-modelling for a “sign and symptom” of high staff turnover (adapted from Agusti, A. (6)).
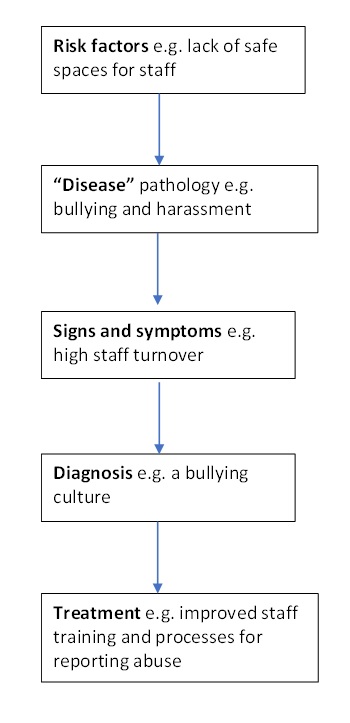
In this conceptualisation, the starting point for culture change is the observation of a sign and symptom in the organisation’s culture (i.e. high staff turnover). This permits investigations (e.g. staff surveys and exit interviews) which facilitate a diagnosis (e.g. a bullying culture) culminating in an appropriate intervention or treatment (e.g. improved staff training and processes for reporting bullying).
By focusing on “pain points” i.e. the signs and symptoms of unhealthy cultures, it is easier to pin-point problems and design interventions/treatments that will help achieve measurable benefits.
Think about it. You wouldn’t prescribe antibiotics to treat a viral infection. So why prescribe branded ‘value-defining initiatives’ (5) to treat organisational ailments that have their own unique pathology?
References
- Arnold J. Work Psychology: Understanding Human Behaviour in the Workplace. 4th edn. London: Prentice Hall Financial Times; 2005.
- West M., Eckert R., Collins R. Caring to change. How compassionate leadership can stimulate innovation in health care. Kings Fund, 2017.
- Kline, R. Leadership in the NHS. BMJ Leader,2019;3:129-132.
- Zubairu, A. Organisational values: a much needed refresh. BMJ Leader blog, 2022.
- Waheed A., Presswood E., Scott G. Organisational values of National Health Service trusts in England: semantic analysis and relation to performance indicators. BMJ Leader,2022;6:192-198.
- Agusti, A. The disease model: implications for clinical practice. European Respiratory Journal, 2018;51:
Author

Ali Raza
Ali Raza is an alumnus of the NHS General Management Training Scheme. Ali has worked on Realistic Medicine in NHS Scotland.
Declaration of interests
I have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.