Human behaviour will determine how quickly covid-19 spreads and the mortality. Therefore behavioural science must be at the heart of the public health response. While responding agencies move quickly to issue advice intended to raise awareness and inform the public and professionals about what actions to take to minimise transmission, behaviour change in the face of a looming pandemic can be slow and may be too late to prevent hundreds or thousands of potentially avoidable deaths. It is important that we learn the lessons from previous incidents and act now to ensure behavioural science is at the centre of the planning and delivery of the public health response designed to mitigate the effects of covid-19. [1]
Experience from previous incidents underlines the importance of ensuring that protective behaviours are delineated and that behavioural advice to the public and health professionals is acted upon. The surge of unaffected patients into medical facilities during the SARS outbreak and the low uptake of the H1N1 vaccine during the 2009/10 pandemic should serve as reminders of this. [2,3] Equally, emergencies such as infectious disease outbreaks can result in spontaneous pro-social and adaptive behaviours in affected populations, which need to be understood and guided. A new pandemic will challenge the capacity of any system; the success of our mitigation efforts will inevitably rely on informal networks of family and community support and care.
For the public, we need to provide actionable information for self-protection and clear guidance for treatment seeking. [4] There is a science behind how to make information “actionable.” The first step is to identify precisely what behaviours are involved—who needs to do what, when, where. The second is to ensure that people have the capability, opportunity, and motivation, to enact the desired behaviours; if any one of these are missing, the behaviour will not occur. [5]
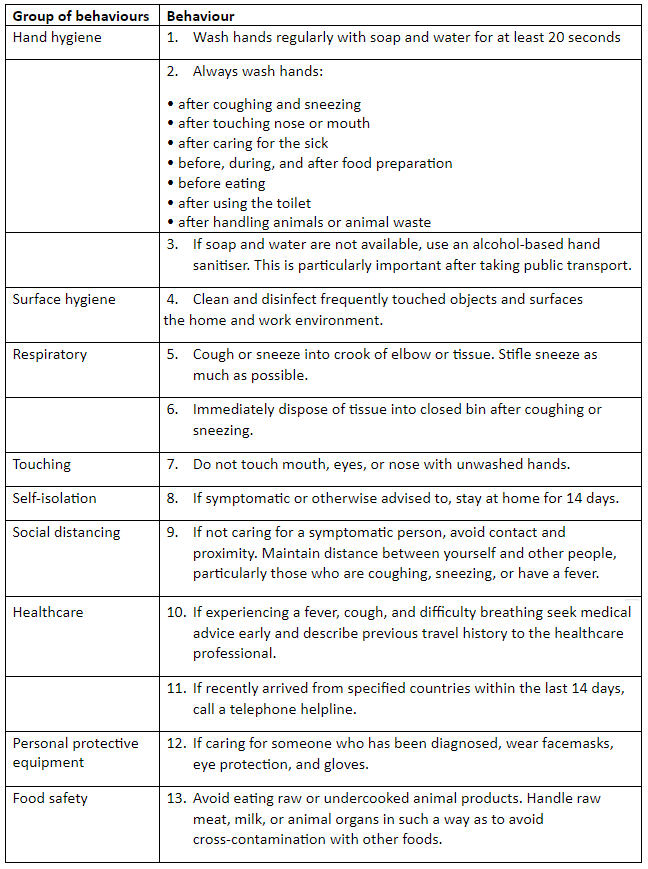
A review of advice from the World Health Organisation, Centres for Disease Control and Public Health England suggests 13 behaviours important to reducing transmission. (Table 1) [6, 7, 8] The relative importance of each behaviour may differ from country to country depending on local context. Each of these behaviours require sub-behaviours that may differ according to situation. Each behaviour involves different challenges in terms of the motivation, capability and opportunity needed to enact them. We must be considering now how to meet these challenges.
As there is much we do not know about transmission of covid-19, continued research is important. The behavioural science research agenda should include study of:
- Current population levels of knowledge, anxiety and trust in responding agencies, attitudes towards COVID-19 public health measures, and the influence of communication strategies on these variables.
- Barriers and facilitators for public health interventions including, for example, adherence to self-isolation protocols.
- Tailoring of information needs for sub-groups, including heterogeneous population groups and health professionals.
- The intended and unintended psychological and social impact of public health and behavioural interventions designed to change transmission-related behaviours (e.g. anxiety, stigma).
- The concerns, intentions and behaviours of healthcare workers.
- The management of uninfected people or those with mild illness, to provide targeted information and reassurance, and prevent unnecessary engagement with health services.
- Changes in contact patterns amongst the general public as a result of information, rumour or public health interventions such as school closures.
- Managing and mitigating the consequences of COVID-19-related absentee-ism and presentee-ism in schools and in the workplace.
In order to prepare the UK population most effectively, to help contain covid-19, and to reduce transmission if it becomes widespread in the future, we need to fully integrate behavioural science into the UK’s public health response.
 Susan Michie is Professor of Health Psychology and Director of the Centre for Behaviour Change at University College London and a member of the Scientific Pandemic Influenza Group on Behavioural Science (SPI-B): 2019 Novel Coronavirus (Covid-19)
Susan Michie is Professor of Health Psychology and Director of the Centre for Behaviour Change at University College London and a member of the Scientific Pandemic Influenza Group on Behavioural Science (SPI-B): 2019 Novel Coronavirus (Covid-19)
James Rubin Reader in the Psychology of Emerging Health Risks, King’s College London
Richard Amlôt is the head of the Behavioural Science Team, Emergency Response Department Science and Technology (ERD S&T) at Public Health England, and visiting professor of practice in the psychology of health protection at King’s College London.
Competing interests: None declared