Speaking in Berlin earlier this year, Angela Merkel reminded world leaders that health is a shared task and that to live dignified lives, we must all collaborate on common goals
 “Those who do not find time every day for health must sacrifice a lot of time one day for illness.” These words of wisdom by Sebastian Kneipp are still relevant today and should be heeded not only by career politicians. Eat healthy, get enough exercise, don’t smoke, have regular medical check-ups and get vaccinated—and here I am referring to a current public debate in Germany that the federal minister of health is strongly, and I must say rightly, engaged in—all this is key to avoiding the diseases of modern society. We know that there is a very close link between living a healthy lifestyle and individual wellbeing.
“Those who do not find time every day for health must sacrifice a lot of time one day for illness.” These words of wisdom by Sebastian Kneipp are still relevant today and should be heeded not only by career politicians. Eat healthy, get enough exercise, don’t smoke, have regular medical check-ups and get vaccinated—and here I am referring to a current public debate in Germany that the federal minister of health is strongly, and I must say rightly, engaged in—all this is key to avoiding the diseases of modern society. We know that there is a very close link between living a healthy lifestyle and individual wellbeing.
Sebastian Kneipp’s helpful advice makes the case for prevention—which should have a permanent and prominent place not only in our individual lives, but also throughout the healthcare sector. Prevention and prudent behaviour by no means apply only to individuals since diseases always have an impact on society as a whole. Dealing with them requires time and money, as well as expertise and medical equipment. It would be an overwhelming task for an individual to provide full personal health insurance. That’s as true for each of us as it is for entire countries and regions—especially those that are not the most affluent in the world.
If you think that developing a healthcare system is a task that stops once you’ve reached a certain development threshold, then think again. We see this every day. If you have visited the poorest countries in the world (and I recently spent three days in Mali, Burkina Faso, and the Niger) then you will have seen the range of issues for which director general of the World Health Organization Dr Tedros is responsible, and how different problems are there compared to our industrialised countries. We must, of course, make sure that we live healthy lifestyles and maintain good healthcare systems. However, we also must contribute what we learn through research and development. For example, we don’t want to promote antimicrobial resistance through bad livestock farming practices that could have a global impact, and we want our development cooperation efforts to help other regions attain sustainable development and health goals. Another cabinet colleague of mine, Gerd Müller, will rightfully be participating in this congress.
Communicable diseases
So health is a shared task, in both a national and global sense. This is especially true and evident for communicable diseases. These can cross borders and have devastating effects. The Ebola outbreak in 2014 in west Africa was a particularly painful reminder of this. Currently, in the Democratic Republic of the Congo, we see how political instability and insecurity due to Ebola are forming a disastrous combination. The disease is being used to assert political interests and aid workers are being threatened and attacked.
In April, such an attack resulted in the death of Richard Mouzoko, an epidemiologist who was on WHO deployment. So it is true that people are sacrificing their lives, or being forced to sacrifice their lives, because in addition to horrible diseases they are caught in the crossfire of political tensions. Dr Tedros, I also want to take this occasion to express our sincere condolences to the family, friends, and colleagues of Richard Mouzoko. It is unacceptable—and we must stand up for the cause—that people who simply want to help others must risk life and limb to do so. After all, the only things stopping the further spread of Ebola are the committed and tireless efforts of aid workers.
Unfortunately, the number of infections recently rose again. That is why I want to use this opportunity to repeat my appeal to all those in positions of responsibility in the region that they give aid workers truly unhindered access, so that current infection numbers don’t grow into an even greater epidemic. I know this is much easier said than done—especially in a region where violent outbreaks are a regular occurrence. However, this also underscores the importance of the MONUSCO mission of the United Nations, which aims to stabilise the Democratic Republic of the Congo.
Of course, the best way to help aid workers would be to have far less need for their assistance—that is, if there were more prevention. Merely reacting to health risks is not optimal—especially when aid efforts are obstructed by security risks, often exactly at the time when help is most urgently needed. This is why we must continue to work together to strengthen the healthcare sector, even at times when health risks do not dominate the world’s headlines. We must prepare international systems as best we can to deal with future emergencies.
Here, I want to say that significant progress has been achieved on coordinating the processes within WHO and the United Nations. I want to thank director general Tedros for his reform efforts, as well as for building a clearly structured system to deal with emergencies. Dr Tedros, this is an area in which we would like to continue providing support. People who are acquainted with this topic will know that, although the words of the director general of a UN organisation do hold sway, at the UN itself the regions often act independently. Many good arguments and lots of persuasion are therefore needed to achieve seamless cooperation.
Collective responsibility
Of course, international agreements do not relieve individual countries of their responsibility. Strengthening national healthcare systems is after all in the vested interest, and incidentally also in the economic interest, of every country because health is a key prerequisite for national economic development. Here, however, I would like to add the following: My visit to Mali, the Niger, and Burkina Faso made clear to me how large the threat of terrorism is in all three countries. They spend between 20% and 30% of their budgets exclusively on security. When that happens, other equally important areas of development are shortchanged. These tasks are therefore very much interlinked—guaranteeing security and providing healthcare services, thereby helping to promote economic prosperity.
Germany makes available more than €1 billion annually in economic cooperation funding for health related projects. Our aim in doing so is to jointly work on finding solutions where they are needed. In this connection, let me say that I very much approve of the WHO approach not to dictate solutions, but rather to travel to the respective regions first to learn what is actually required and what actions will have a lasting effect. For example, it would not make sense to build entire hospital sites at an arbitrary location without also making sure that the respective infrastructure and links are also ensured. That is why cooperation through partnerships is urgently needed to create both acceptance in these regions and to achieve lasting, desired results.
Whether the goals be humanitarian objectives, development policy aims, economic interests, or even self-motivation—we must act to limit the spread of diseases. For everyone in the international community, this is a shared responsibility. We have a duty to support poorer countries, so that they can live up to their responsibilities.
This shared responsibility is also reflected in the 2030 agenda for sustainable development. In Germany, we are committed to the sustainable development goals (SDGs). That, after all, is what’s special about the SDGs: rather than targeting the less developed countries, they are part of a joint, global agenda. We have considerably stepped up our engagement on SDG 3—not only financially. Hermann Gröhe has just said that we very deliberately placed this issue on our G7 and G20 presidency agendas, and we’ve done everything we can to make sure that it is not forgotten.
I’m therefore most grateful to Japan, which holds the current G20 presidency, for focusing on the issue of universal health coverage. We want to talk about how we can obtain agreement on substantial steps towards universal health coverage. The heads of state and government will also talk about this at the United Nations in September. This will send a very important signal, because we will thereby be highlighting the importance of global and universal health coverage.
Health issues are one of the areas where international cooperation can show what it’s capable of. An example that occurs to me is the Pandemic Emergency Financing Facility of WHO and the World Bank. They are very valuable instruments to make crisis management funds available swiftly and without red tape. In fact, we simulated our health emergency coordination capabilities with an exercise during our G20 presidency. The German government is very active in this regard.
Sharing knowledge and resources
In my opinion, it is just as important for research progress to also benefit countries with weaker economies. Thanks to the CEPI alliance—the Coalition for Epidemic Preparedness Innovations—we can more effectively deploy new vaccines, and with the Global Antibiotic Research and Development Partnership we can efficiently and fairly distribute new antibiotics. Possibly one of the most serious problems we have (although it is often underestimated) is that we often prescribe antibiotics too liberally. It is incredibly difficult and by no means certain that we can constantly develop new antibiotics. This is why we must act very prudently and carefully.
Research often does not devote enough attention to many diseases in poorer countries and the ways that they can be treated because of the bottom line. There is a significant danger that rich countries will work on addressing their diseases and at the same time overlook the fact that, in other places, there are widespread diseases for which real treatment progress could be achieved with modest investments in research. It is a matter of particular importance to me that we not forget such poverty related diseases. According to estimates, these affect more than one billion people. So called neglected tropical diseases are therefore by no means negligible.
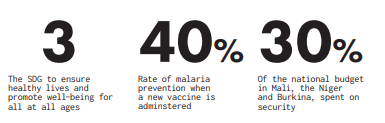
This is of course true for the “big three” of HIV/ AIDS, malaria, and tuberculosis. In Africa alone, some 250 000 children still die from malaria every year. Knowing what a malaria net costs, and giving some thought to the idea of supplying these, it becomes obvious that we really should take action wherever we can. To combat these diseases, we have the Global Fund, which is due to be replenished for the years 2020 to 2022 this October in Lyon. Germany will again make a substantial contribution. Much hope is being placed in the new malaria vaccine. It is being tested in Malawi, took three decades to develop, and has the potential to prevent 40% of overall cases and 30% of severe cases of malaria. It would be significant progress if we could actually get this vaccine out to where it is needed.
Health and the 2030 agenda
I think the examples I’ve given prove that health alone is worth all the effort that we can devote to it. But there are good reasons that one of the sustainable development goals for the 2030 agenda is health and wellbeing. This shows that health is intricately interconnected with other SDGs that affect the wellbeing of each and every one of us.
Considering the key role of health for a dignified life, I have joined Norwegian prime minister Erna Solberg and Ghanaian president Nana Akufo-Addo in calling for a plan of action to implement SDG 3. I’m very grateful for the committed efforts of WHO in this regard. Dr Tedros, this work is very important, and we will continue to support it. If we know what specific measures can help accelerate progress towards, or just help achieve, health related goals, then we can take more targeted action.
That, after all, is key to delivering on all the goals of the 2030 agenda for sustainable development. Just think: there is a large number of recipient countries—there are more than 50 countries in Africa alone. And there are certainly 60 or 70 countries that are able to provide aid for development measures. Yet no one looks at the combined effect—that is, how efficiently goals in the respective country are being met. It is therefore paramount, and WHO indeed does this, to internationally coordinate action. We must pay attention to what assistance is given where, and to how we can make sure that we are on the right track to achieving the SDGs.
A plan for action
At the World Health Summit last October here in Berlin, a first version of the plan of action was presented. Work on drafting the final version is under way. That will certainly also be one of the topics of discussion here today. Initial results show that the signatory organisations—such as WHO, UNICEF, the World Bank, the Global Fund, and Gavi, the Vaccine Alliance—are comparing and aligning their programmes of work and unifying their strategies. I am very much looking forward to the final document, which is due to be presented during UN Week in September. Maybe Dr Tedros will give us some examples of these efforts. Of course, we also make a point of working with foundations. The Bill and Melinda Gates Foundation, for example, is represented here today, and representatives of other foundations may be here as well. Here, too, we must make sure that activities to reach our goals are coordinated.
I certainly hope—and here I turn to the head of my parliamentary group—that the German Bundestag will be of assistance in this regard. I would welcome it if our parliaments could help lobby support for the action plan because it is very important. The fact that a subcommittee on global health was newly established this legislative term, is also a sign that we believe the time has come to again focus on this issue. I am pleased that there is broad consensus on this topic.
That of course is also very important for us in the German government. We know that our budget will be slightly lower this year, maybe also next year. However, we hope that the issue of global health will remain a top priority. I assure you that the German government will remain strongly engaged on this issue. We are working on a new strategy that we intend to present before the end of the year.
Finally, I would like to say that every person on earth should be able to live a healthy life. In poorer countries, people must still be given access to a functioning healthcare system. With the 2030 agenda, we made a strong commitment. We are, however, bound not only by the document, but above all by the human imperative. We can accomplish great things by acting as one. I am convinced that today’s congress is helping to raise the profile of this issue, and that through coordinated joint action we can make even better progress towards the ambitious goals that we have set.
A speech by federal chancellor Angela Merkel at the congress organised by the CDU/CSU parliamentary group on Strengthening Global Health—Implementing United Nations SDG 3 held in Berlin on 8 May 2019. Reprinted with permission.
First published in Health: A Political Choice, an official Global Governance Project publication, edited by John Kirton and Ilona Kickbusch. Read your copy here www.bit.ly/2019UHC
Angela Merkel is the chancellor of Germany. Twitter: @AngelaMerkeICDU
