What makes a good definition? There are five guidelines:
• A good definition describes all the essential attributes of the definiendum, the thing being defined. To define something (Latin definire) is to determine its boundaries (Latin fines), and hence to state exactly what the thing is or to set forth or explain its essential nature; this is what Aristotle called τό τί ἦν εἶναι (literally, that which is). Thus, a definition is “a precise statement of the essential nature of a thing” (Oxford English Dictionary).
• It must not be too wide or too narrow. As its etymology implies, a boundary must be drawn round a definition so that it includes everything essential and excludes everything inessential.
• It should avoid circularity. For example, to define a medication error as “any error occurring in the medication process” is circular, since what it says, in effect, is that a medication error is an error in medication.
• It must not be obscure. The words used in a definition must themselves be easily understood without further definition. When defining technical terms it may be hard to comply with this.
• It should, if possible, be positive not negative. One should not, for example, define “wisdom” as “the absence of folly”; after all, there are many other things one could put in place of “folly” here. Negative definition also encourages circular definition; having defined “wisdom” as “the absence of folly, one might, for example, define “folly” as “the absence of wisdom”.
Occasionally, the last of these guidelines may be legitimately ignored. For example, when two categories can be clearly distinguished and carefully defined, one of them can reasonably be described as the negation of the other. Examples include invasive and non-invasive treatments, coding and non-coding RNA, obese and non-obese individuals, and communicable and non-communicable diseases.
In some cases specific diseases can be similarly labelled. For instance, when only two viruses that caused viral hepatitis had been identified, hepatitis A and hepatitis B, other cases of viral hepatitis, in the absence of evidence of a causative agent, were called non-A non-B hepatitis, recognizing that other unknown viruses might be responsible. Later, in the 1970s, when other viruses were identified they were called hepatitis C, hepatitis D, and so on. Since then the term ”non-A non-B” has gradually fallen out of use (Figure 1).
![Numbers of papers containing the term “non-A non-B [hepatitis]” since its first appearance in 1975](https://blogs.bmj.com/bmj/files/2018/08/aronson_non-diseases.png)
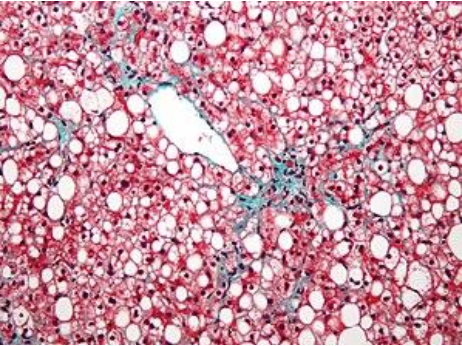
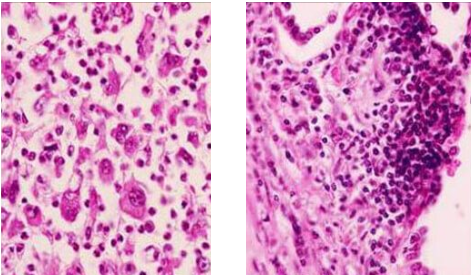
Likewise, non-small cell lung cancer contrasts with the small cell variety (Figure 3). The former is considerably more common than the latter and is heterogeneous, encompassing adenocarcinomas, squamous cell carcinomas, and large cell carcinomas. Furthermore, non-small cell carcinomas have polymorphisms in genes such as the anaplastic lymphoma kinase (ALK) gene, which may predict responsiveness to specific agents, such as crizotinib and ceritinib, in small numbers of individuals.
Other examples of heterogeneous conditions negatively defined include non-valvular atrial fibrillation, non-neural granular cell tumours, and non-Hodgkin’s lymphoma.
Negative definitions of heterogeneous groups of diseases are useful insofar as they hide ignorance and make no assumptions about their pathologies, but they should be replaced by definitive descriptions when their heterogeneity is understood.
 Jeffrey Aronson is a clinical pharmacologist, working in the Centre for Evidence Based Medicine in Oxford’s Nuffield Department of Primary Care Health Sciences. He is also president emeritus of the British Pharmacological Society.
Jeffrey Aronson is a clinical pharmacologist, working in the Centre for Evidence Based Medicine in Oxford’s Nuffield Department of Primary Care Health Sciences. He is also president emeritus of the British Pharmacological Society.
Competing interests: None declared.
