We are all asked for feedback. We all receive feedback and then feedback on the feedback. This almost obsessive behaviour with feedback, in many cases, means the emphasis on the actual content of the original feedback is somewhat lost.
As a training doctor in the UK, I am often asked for various reports on my progress: both reports completed by myself and reports completed by a selection of colleagues.
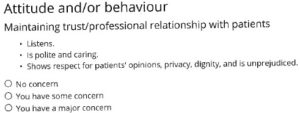
I was looking forward to discussing my latest feedback with my ARCP (Annual Review of Competence Progression) appraiser, as I was confident with the efforts and progression I had made. It was therefore somewhat surprising and disappointing to realise that the feedback was designed only for raising major concerns.
Discussing this with hospital colleagues and reading blogs on the subject, I have come to realise that the way junior doctor feedback is designed reflects the current state of the NHS. We are treading water, staying afloat. Don’t drown, and you won’t be picked up.
But what about those who want to excel? How does the current system encourage excellence? At what point did we lose the scope for aiming for the highest possible standard? It is demoralising to think that “no concern” is the level we now aim for. I want to understand how one might achieve more than simply “no concern.”
In a service blighted by problems with funding, politics, and staff shortages, it is unfortunate that, within the job, there is not the incentive between professionals to reward striving for excellence. If we don’t suggest it and encourage it in our newest trainees, what kind of future do we envisage for medicine?
Hannah Wilson is an academic junior doctor at Imperial College NHS Trust, London. Her interests are in education and training in medicine
Competing interests: none declared
Further reading:
Making junior doctors’ lives easier
Trainees dissatisfied with “tick box” ARCP, researchers find