We need to talk about patients not pounds if we are to engage clinicians in meeting the NHS productivity challenge. That means focusing on providing the best possible health outcomes at the lowest possible cost, rather than a single-minded push to save money.
We need to talk about patients not pounds if we are to engage clinicians in meeting the NHS productivity challenge. That means focusing on providing the best possible health outcomes at the lowest possible cost, rather than a single-minded push to save money.
This is one of the main messages from our new report, Better value in the NHS: the role of changes in clinical practice, and was the main topic of discussion at The King’s Fund conference on better value healthcare. At that event, Sir Muir Grey put the issue more succinctly by asking the audience to join him in instigating a ban on the word “savings.”
Past performance shows we need a new approach. Since the 1980s, NHS productivity – that is outputs (activity) divided by inputs (physical inputs, mainly staff) – has increased by around 1 per cent a year on average. That figure has been higher over the past five years but this has been mainly due to the freeze of NHS wages and real-terms reductions in the tariff price paid for services. These centrally driven measures cannot slice much more from NHS budgets, as demonstrated at the end of last year by the first pay-related strike action in the NHS for 30 years (we await the NHS reaction to the latest pay deal announced in the budget) and re-emphasised this year, when the majority of NHS providers rejected proposals for the reduced 2015/16 tariff for hospital services. To get anywhere near the 2–3 per cent annual productivity growth required to meet the £22 billion productivity challenge set out in the NHS five year forward view will require clinical teams to find ways to improve the quality of their services and get more value from every pound spent on health.
The link between quality and cost is complex. A large review of the evidence on whether quality-improvement interventions saved money for health care providers found mixed results; some interventions (often those on a small scale) resulted in quality improvements and reduced costs but others (particularly those on a large scale) failed to do so. While this paints a fairly pessimistic picture for those seeking to deliver better value care, looking at what NHS clinical teams are doing on the ground to redesign their services tells a very different story.
In Walsall, commissioners, pharmacists and GPs have improved patient care and saved money by introducing a pharmacist-led repeat-prescription service. The 200+ prescriptions that GPs had to authorise each week are now managed by pharmacists, who – among other things – eliminate duplicate medications, switch patients from branded to chemically identical generic drugs, and address any issues patients have taking their medicines. By reducing over-ordering and wastage this service generated more than £800,000 of savings in 2014/15, a return of £3.54 for every £1 invested. Additionally, medications are better managed, there are fewer prescribing errors and GPs have more time to focus on patient care. Read more about this case study in the full report.
At Plymouth Hospitals NHS Trust frontline staff have also managed to improve quality and cut costs. They analysed patterns of activity in their acute stroke unit and identified a group of frail older patients who had had severe strokes who consumed the highest proportion of their resources and were having a particularly poor patient experience. They redesigned the care pathway for these patients by adding daily reviews of their care and a range of different treatment options. Within a year, transfers to the stroke unit were happening 12 per cent faster and the average length of stay had fallen by 6 per cent. This allowed 13 acute and 4 rehabilitation beds to be permanently closed and saved an estimated £1,000 per patient. Read more about this case study in the full report.
The NICE local practice collection has many more examples like these from different parts of the country and of the health system. Despite their diversity these innovations have a number of things in common:
- they were driven by frontline teams who know best how to improve their services
- they managed to improve the care that patients receive and save money
- they showed results relatively quickly – often within a year.
- This leaves us with one obvious question: how can the creativity and success shown in these examples be spread across the country?
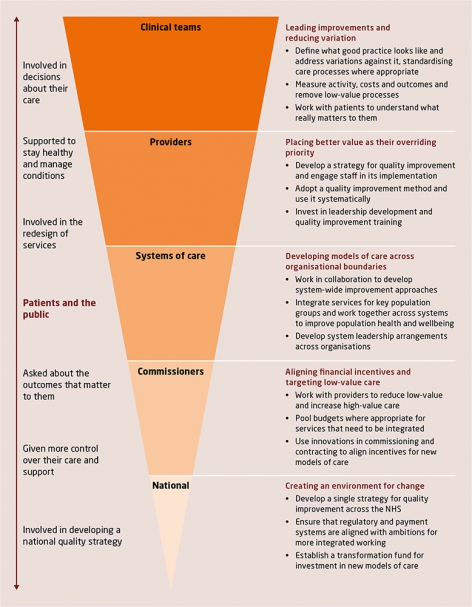
There’s no simple answer to that question, but in our report we make a start by outlining an agenda for action. We put clinicians at the top of the pyramid as they must be the powerhouse behind improvement in the NHS. However, action will be needed across the health service to create an environment that gives clinical teams the time and space to transform services. And patients must be involved at every level too, from decisions about their own care to the design of a national quality strategy.
We need to shift the debate on productivity to focus on delivering better value care for patients. Unless we do, the value-driven clinical community will not engage with the challenge of transforming services in a time of tight budgets – and the NHS cannot meet its current and future challenges without them.
Ruth Robertson is a fellow in health policy at The King’s Fund.
This blog first appeared on the King’s Fund website here.