By Jamie Carlin Watson
Increased understanding of social determinants of health and health literacy have expanded the responsibilities of the medical community from patients in the clinic to citizens at increased health risks. Fulfilling these responsibilities involves, in part, distributing timely and accurate health information that is accessible, understandable, and usable.
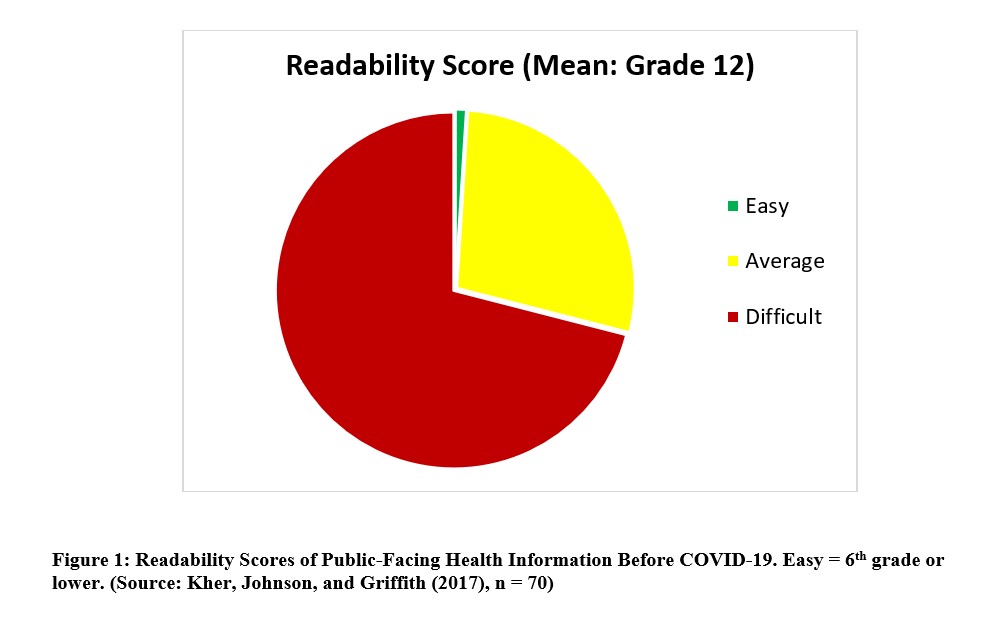
Though increased commitment to using plain language and developing decision aids holds some promise for improving medicine’s role in public health, public-facing health information still falls far below what health communication scholars regard as acceptable for people who struggle with health literacy. For example, Kher, Johnson, and Griffith (2017) found that, of 70 public-facing health documents on heart failure, 99% averaged higher than the recommended “easy” readability level, which is sixth grade or lower (Figure 1).
During public health emergencies, the primary ethical orientation of medicine shifts from individual patients to populations, thus increasing the medical community’s responsibility to provide the public with needed health information. COVID-19 presents a special problem in this regard, as certain populations at increased risk of contracting and experiencing the worst effects of the virus are also at risk for inadequate health literacy.
Health communication researchers find that Black and Hispanic Americans and people over 65 are at higher risk of inadequate health literacy than their white counterparts (here; here; here). And all three populations experience a disproportionately high rate of infection and death rate from COVID-19 (here; here; here).
Unfortunately, public-facing health information about COVID-19 fares little better than its pre-COVID-19 counterparts. Alison Caballero, Katie Leath, and I at the Center for Health Literacy at University of Arkansas for Medical Sciences recently conducted a study of 28 public-facing health information documents about COVID-19, and we found that these documents were only marginally better than public-facing materials before the pandemic, with 93% averaging above the “easy” level (Figure 2).
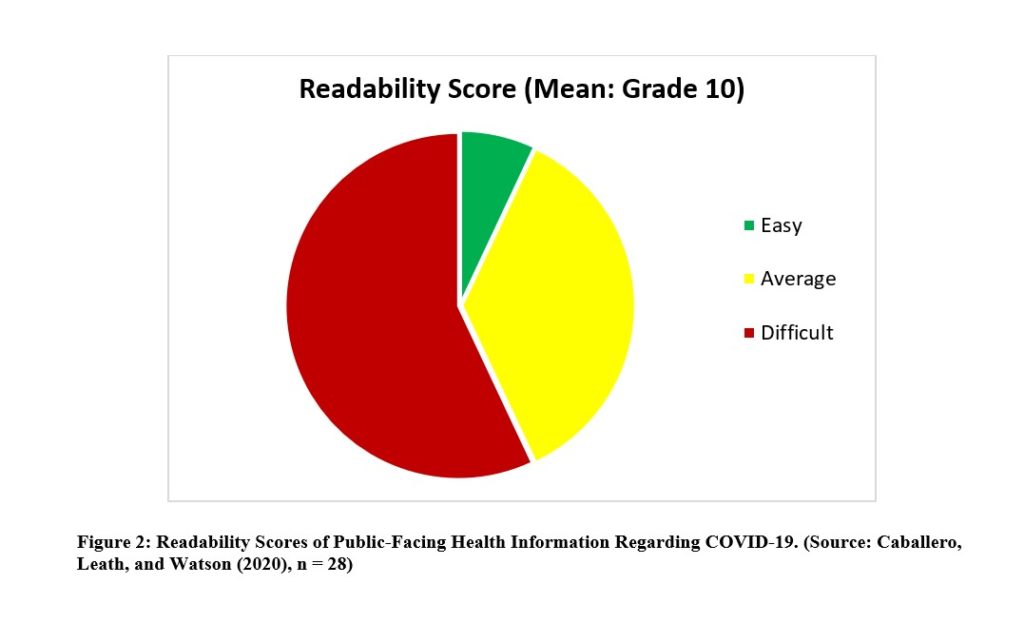
Kher, Johnson, and Griffith claim that their data shows that 7.1% of their materials were easy and 92.9% were average or above average, which would mean that their results are virtually identical with ours, and so their graph should look much like ours. However, their published data suggests that their documents scored slightly worse than they explain. My rendering suggests that COVID-19 information is slightly better than pre-COVID-19 health information, though the improvement is marginal.
Further testing using the Patient Education Materials Assessment for Print Materials (PEMAT-P) showed that these materials tended not to make their purpose completely evident (58% did), tended not to use visual aids to make content easier to understand (39% did), and tended not to explain actions using manageable steps (61% did). It is also noteworthy that, on most documents, the only actionable step was to click to another website for more information.
These results highlight a failure of public health ethics. Materials that could help reduce health disparities during a public health emergency where accurate information is paramount contribute to barriers for higher risk populations.
But the results also highlight an opportunity for ethicists to partner with health communicators to improve medicine’s impact in the community. Combining insights from public health ethics and health literacy research, health communicators can more effectively develop strategies for minimizing barriers to needed health information.
For example, health communicators can develop templates with commonly needed health information that have been vetted to meet health literacy standards, such as including a clear purpose statements, eliminating or defining jargon, chunking information, creating visual aids, and enumerating specific action-steps. To determine which content is relevant to at-risk populations, and which to give priority, they can organize community focus groups to elicit feedback on these materials.
Further, communicators can make explicit when information is uncertain or likely to change, and direct readers to check back or sign-up for an email list to receive updates. Because there are systemic barriers to trust in health care, health communicators can expressly address skepticism and suspicion, citing independent and easily accessible sources.
Finally, to distribute information, they can partner with community groups, such as churches, senior centers, and social clubs to develop messaging that directly addresses the concerns of at-risk populations. And health communicators who have the ear of public health officials can offer to improve health communications, such as reviewing information for plain language and ensuring that all materials are available in all needed languages in a community.
Public health emergencies are not a new phenomenon. And COVID-19 has shown that health communication practices are not adequate for addressing the information needs of communities when they happen. Identifying and understanding the ways that health communication increases risks for already disadvantaged populations can inform strategies for minimizing those risks.
Author: Jamie Carlin Watson
Affiliations: Medical Humanities and Bioethics, University of Arkansas for Medical Sciences (UAMS), UAMS and Arkansas Children’s Hospitals, and Center for Health Literacy at UAMS.
Competing interests: None declared.