By Dominic Wilkinson @Neonatalethics and Julian Savulescu @Juliansavulescu
This week, doctors in France are reported to be withdrawing life-prolonging treatment from Vincent Lambert, a 42 year old French psychiatric nurse, who has been at the centre of a long-running legal battle over his medical treatment.
Lambert was seriously injured in a motorcycle accident in 2008, and has been diagnosed as being in a persistent vegetative state. Since 2014, his case has been heard multiple times in French and European courts. His wife, who is his legal guardian, wishes artificial nutrition and hydration to be stopped and Vincent to be allowed to die. His parents are strongly opposed to this. In May, the parents succeeded in a last minute legal appeal to stop Vincent’s doctors from withdrawing feeding, pending a review by a UN Committee on the Rights of Persons with Disabilities. Then, last week, the French Cour de Cassation overturned the lower court ruling, allowing Lambert’s doctors to reinstitute their plan to sedate Lambert and withdraw treatment. If that plan proceeds, it appears likely that Lambert will die in the coming 1-2 weeks.
This case has obvious parallels with the case of Terri Schiavo, who died in 2005, but there have been other similar high profile cases, over more than forty years in various countries including US, England, and Italy.
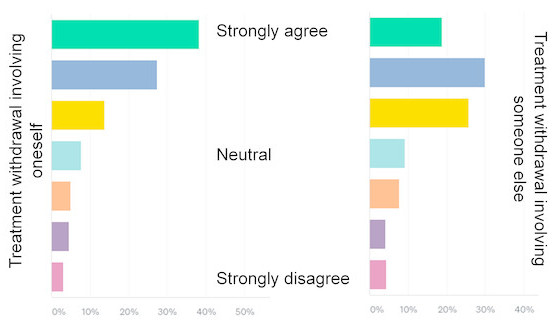
The public in France are apparently divided by the Lambert case. That is not surprising. A recent international survey of the lay public found that 49% agreed or strongly agreed with withdrawal of treatment, while 9% disagreed.
The recurrent nature of debate over treatment for patients in a vegetative state suggests that it is unlikely that our communities will reach a common view on this contentious ethical issue. There then becomes a question about how to deal with the issue of ethical disagreement. Recently, following another controversial example of disputed treatment (the Charlie Gard case), we proposed a ‘dissensus’ framework that might be applied in such cases. In a forthcoming paper in the Journal of Medical Ethics, we examine the implications of dissensus for debates about treatment for patients like Vincent Lambert.
Briefly, while it is valuable to seek consensus about how we should respond to important issues in medical ethics, in situations of deep normative disagreement, it is often clear that consensus is not likely to be possible. In those situations, we must make decisions despite disagreement.
We outline three separate steps to the dissensus approach:
First, it is important to separate out questions of individual benefit (best interests/harm) from questions of collective benefit (resource allocation/distributive justice).
Second, we need to identify the range of reasonable disagreement about options that may be of benefit/harm for the individual – in this case Vincent Lambert. We argue that there is no need to collectively agree about what would be best for Vincent. It is clear that within the French public people have different views about what should happen. Some people read of his case and react with horror at the idea of being kept alive indefinitely in a state of complete dependence and lack of awareness. Other people have the opposite response. They respond with outrage at the idea of stopping feeding and allowing to die a profoundly disabled man, who does not appear to be suffering.
The best ethical response to reasonable disagreement in cases like that of Vincent Lambert is to make decisions based on his values and his wishes. If Vincent himself would not have wished to remain alive, then the wishes of other family members, or politicians, or religious leaders are not relevant. Treatment should be withdrawn.
However, we point out that we need a different approach to issues of collective benefit and resource allocation. While there may be (is highly likely to be!) reasonable disagreement about allocating resources, there is a need to collectively agree about options that represent a limited resource, and may harm others if provided (or reduce available options to others).
Of relevance, in the UK, it is estimated that the nursing home care for patients in a persistent vegetative state costs £90,000-120,000 per year. Derick Wade has pointed out in a previous paper in the journal that this value is considerably in excess of the £20-30,000 cost/QALY threshold commonly used for deliberations about providing novel therapies in the NHS.
There are, of course, difficult questions for our communities to answer about how much we spend on healthcare, how we allocate resources, how we ration medical treatment and whether/when we may discriminate between patients in provision of care.
Our aim in the paper is not to settle those debates. Rather, this analysis suggests that in vexed disputes about treatment for patients like Vincent Lambert the most important question to address may be different from the one that is most commonly the focus of ethical attention.
Paper title: Current controversies and irresolvable disagreement: the case of Vincent Lambert and the role of ‘dissensus’ FREE – OPEN ACCESS
Authors: Dominic Wilkinson1,2,3 Julian Savulescu3,4,5
Affiliations:
- Murdoch Children’s Research Institute, Melbourne, Australia
- John Radcliffe Hospital, Oxford, UK
- Oxford Uehiro Centre for Practical Ethics, Faculty of Philosophy, University of Oxford, UK
- University of Melbourne Medical School, Melbourne Australia
- University of Melbourne Law School, Melbourne, Australia
Competing interests: The authors have no conflicts of interest.
Social medica accounts of authors: Dominic Wilkinson @Neonatalethics Julian Savulescu @Juliansavulescu