The social roots of psychiatric illness are more numerous than has been recognised, argue Kamaldeep Bhui and Jeremy Coid
The link between urban environments, trauma and deprivation, and higher incidence rates of psychosis—generally, but particularly in ethnic minorities—is well established. [1][2][3][4]
GPs, psychiatrists, and mental health and social care professionals working in deprived urban areas witness this connection on a daily basis, and recognise it as a challenge to the provision of comprehensive care.
Ethnicity is often used as an explanation for the higher incidence rates of psychosis observed in deprived areas. Yet our recent analysis comparing data from Hackney (a deprived inner London borough with a diverse range of ethnic minorities) with data from across the country challenges this view.
Our study, which was published last month in the British Journal of Psychiatry, compared the diagnosis rates for psychosis among black, south Asian, and white men across Britain. After allowing for socioeconomic factors such as social class and unemployment, the significant gap between the first two groups and white men disappeared. This would suggest it is these factors that account for the ethnic differences in prevalence of psychosis.
However, when we studied data from an additional group of men living in Hackney, a different picture emerged. After allowing for those same socioeconomic factors, black and south Asian men in the borough still had higher psychosis rates than their ethnic counterparts elsewhere in the country and their white male neighbours.
The gap only disappeared when we assessed the data against four other factors, which were drug and alcohol dependence, criminality and violence, risky or coercive sexual behaviour, and anxiety. Diagnosed levels of psychosis were much more severe among men in Hackney who engaged in such behaviours or were affected by anxiety—particularly when more than one featured in their lives.
These four factors seem to form a “syndemic” with psychosis. The new theory of “syndemics” attempts to explain how different disorders and health behaviours cluster and increase the risk of further disorders in highly deprived areas. A syndemic approach shows how multiple adversities and disadvantages can exacerbate each other, and increase a person’s likelihood of developing a particular condition or group of conditions. Most of this risk might track back to early life experiences that generate poorer health and poorer social and behavioural outcomes, which all seem to interact. With our study we tested (for what we believe is the first time) whether syndemics might be a better way to assess the cause of psychiatric disorders.
Our study has implications for public health, social care, and policing/criminal justice approaches in deprived communities. It also suggests that the syndemic approach—pioneered during the response to HIV/AIDS and latterly used with diabetes—could be employed to great effect in mental health research. The approach fits the idea that there are complex and multiple drivers of mental illness—an idea borne out by what we see in clinical practice and the emerging research. Prevention and care should reflect this.
Our findings suggest that in some deprived communities there are additional challenges and social disadvantages for black and south Asian men on top of deprivation. It is possible that adverse early childhood experiences and other social challenges may be relevant. These experiences are hypothesised to cluster in specific geographical areas. The concept of “place”—which has come to the fore in local government and social policy over recent years—matters.[5] We think that there is a strong argument to be made that place should be seen as a risk factor in the development of psychosis for black and south Asian people.
The experience of generations of multiple disadvantages or challenges should be addressed by policymakers and those commissioning and delivering a range of public services. We need place based measures and interventions in early life that could reduce the risk of later serious mental health problems. Such measures could avoid the need for costly support and, arguably, coercive care (including assertive and compulsory treatments in the community and as inpatients) in later life.[6][7]
GPs and other clinicians increasingly take into account their patients’ economic circumstances when making diagnoses or referral and treatment decisions. We would suggest that they also consider the impact of issues such as anxiety, violence (for example through gang membership), and risky behaviours when evaluating the mental health of their patients in certain geographical areas.
Of course, that might be difficult in hard pressed primary care and mental health settings, yet preventive efforts are known to be cost effective over the life course, especially if applied early in life. The government’s cuts over the past decade to essential (and cost effective) public health services, such as drug and alcohol treatment teams, violence prevention in a public health framework, and sexual health, will also impede attempts to create place based responses.
While we focused on a single London borough, it is likely that these findings are relevant to a number of inner city urban areas with similar demographics and engrained social problems.
The extent of the social roots of “psychiatric illness” has been debated for generations, but we would argue that those roots are more numerous than has been recognised. Further studies involving a syndemic approach would help us better identify the many causal influences on mental health and how they interact. Once we understand this, we’ll be in a stronger position to identify preventive opportunities.
 Kamaldeep Bhui is a professor and head of the Centre for Psychiatry at Queen Mary University of London. He is also an honorary consultant psychiatrist at East London NHS Foundation Trust, the former public health lead and now chair of the Publications Management Board at the Royal College of Psychiatrists, and editor in chief of the British Journal of Psychiatry. Twitter @KSBhui
Kamaldeep Bhui is a professor and head of the Centre for Psychiatry at Queen Mary University of London. He is also an honorary consultant psychiatrist at East London NHS Foundation Trust, the former public health lead and now chair of the Publications Management Board at the Royal College of Psychiatrists, and editor in chief of the British Journal of Psychiatry. Twitter @KSBhui
Competing interests: None declared.
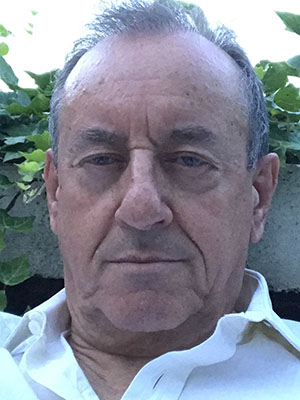 Jeremy Coid is a professor of epidemiology in psychiatry at West China Hospital, Sichuan University, China and emeritus professor of forensic psychiatry, Queen Mary University of London, UK. He was director of the Violence Prevention Research Unit at Queen Mary and a member of the WHO Violence Prevention Alliance. He was a consultant forensic psychiatrist in East London for 30 years.
Jeremy Coid is a professor of epidemiology in psychiatry at West China Hospital, Sichuan University, China and emeritus professor of forensic psychiatry, Queen Mary University of London, UK. He was director of the Violence Prevention Research Unit at Queen Mary and a member of the WHO Violence Prevention Alliance. He was a consultant forensic psychiatrist in East London for 30 years.
Competing interests: None declared.
[1] Coid JW, Kirkbride JB, Barker D, Cowden F, Stamps R, Yang M, et al. Raised incidence rates of all psychoses among migrant groups: findings from the East London first episode psychosis study. Arch Gen Psychiatry 2008;65(11):1250-8.
[2] Stanton KJ, Denietolis B, Goodwin BJ, Dvir Y. Childhood Trauma and Psychosis: An Updated Review. Child Adolesc Psychiatr Clin N Am 2020;29(1):115-29.
[3] Coid JW, Zhang Y, Li T. Urbanicity and Psychosis. JAMA Psychiatry 2018;75(12):1301.
[4] Halvorsrud K, Nazroo J, Otis M, Brown Hajdukova E, Bhui K. Ethnic inequalities in the incidence of diagnosis of severe mental illness in England: a systematic review and new meta-analyses for non-affective and affective psychoses. Soc Psychiatry Psychiatr Epidemiol 2019.
[5] Schofield P, Das-Munshi J. New directions in neighbourhood research-a commentary on Lovasi et al. (2016): Cause and context: place-based approaches to investigate how environments affect mental health. Soc Psychiatry Psychiatr Epidemiol 2017;52(2):135-7.
[6] Barnett P, Mackay E, Matthews H, Gate R, Greenwood H, Ariyo K, et al. Ethnic variations in compulsory detention under the Mental Health Act: a systematic review and meta-analysis of international data. Lancet Psychiatry 2019;6(4):305-17.
[7] Halvorsrud K, Nazroo J, Otis M, Brown Hajdukova E, Bhui K. Ethnic inequalities and pathways to care in psychosis in England: a systematic review and meta-analysis. BMC Med 2018;16(1):223.
