 The situation is clear. The child has an illness which is very likely to end their life – and soon – in days, not months or years. They may be hooked to a ventilator, drizzled with inotropes, or osmosed. The health care team is talking – once again – about the outcomes and what we can, should or will do.
The situation is clear. The child has an illness which is very likely to end their life – and soon – in days, not months or years. They may be hooked to a ventilator, drizzled with inotropes, or osmosed. The health care team is talking – once again – about the outcomes and what we can, should or will do.
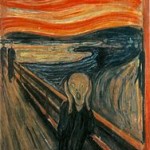
Do you recognise this?
Do you recall how people spoke – not the ~mab, the pressor or the particular hospice name – but what the emotional and moral content of the discussions were? Can you recall if that varied between professional groups & experience of those folk? And if there were clashes between how people felt the actions should flow, against how they were made to act?
This is the question that has been investigated by a new systematic review in the ADC, drawing together original papers who have enquired about ‘moral distress’ in NICU / PICU
The group undertook a complex, multilayered search (Find) to discover papers that might have been relevant, cut into them to see how well they were made using an appraisal system (Appraise) and involved this in the summary. To cut to the chase, they found 13 studies, all relatively small, and only 5 multiprofessional. The way the synthesis took place was by a simple thematic analysis, the most basic form that can be used, though the analysis could potentially have been undertaken with a more complex approach.
Now I am aware that a key part of standard critical appraisal training is “don’t read the discussion” … but in quite a lot of papers, qualitative synthesis in particular, the discussion is actually part of the scholarship rather than part of the sales pitch. In this they summarise the transferability key messages:
[they tell us the] causes of moral distress, relational dynamics between healthcare professionals within different settings or ethical climate and the impact of moral distress over time
The causes of moral distress seem to be the clashes between interventions undertaken and the benefits that could occur, potentially not in the best interest of the child, and a lack of ability to ‘do the right thing’. The relational dynamics that flow into this include the perception of medics as pressing on with life-saving treatments, and nurses caring deeply and personally for the child and family – but this is probably not really true – and reflects the way research has been undertaken, the way the instruments to judge ‘moral distress’ don’t work in medics, and the medical use of different language – “dilemma” and “confrontation” – despite the presence of an internal crash of ideas that is moral dilemma.
What do we know about what happens over time? Well moral distress may lead to burnout & leaving jobs. Experience / age may reduce the experience of moral distress. Lots of may. Not a lot of know.
Does it matter? Is this a pointlessly academic – socialologically soused – barrel of work that does nothing in the world? I don’t think so – I think we under play the internal agonies we have at work – and we need to be aware of burnout and keep safe those who are at risk. Understanding the mechanisms of these ‘pathologies’ should be considered as important as other pathologies, like bronchiolitis, COPD and psoriasis.
– Archi