Authors:
Nikki Pease, Consultant in Palliative Medicine, Velindre Cancer Centre, Cardiff, Wales
Mark Taubert, National Strategic Lead for Advance/Future Care Planning, NHS Wales
Introduction:
“Shared Decision making should also include an ability to share the decisions that have been agreed on”
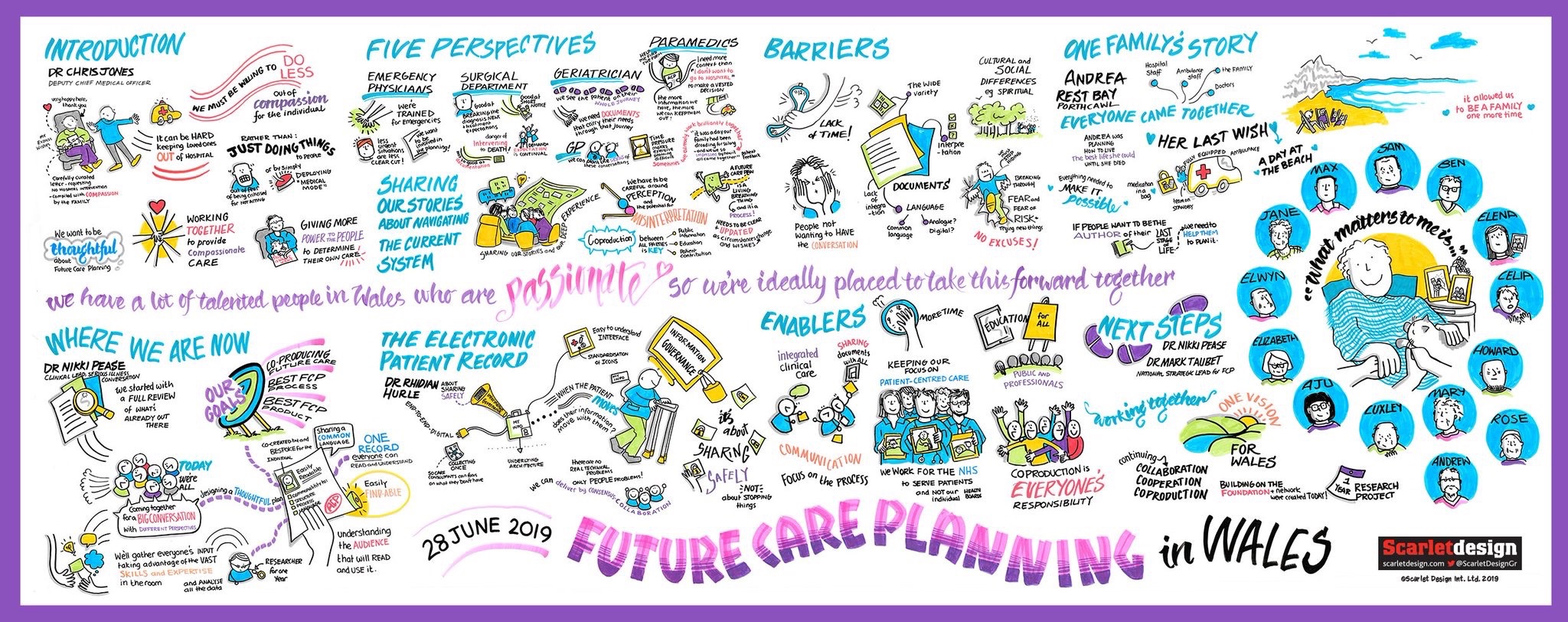
In 2019, BMJ Supportive & Palliative Care featured a write-up of the proceedings of a national conference on Future Care Planning in Wales. ‘Future Care Planning‘ (FCP) was introduced within NHS Wales as an umbrella term to encompass both Advance Care Planning, which, by definition [1] involves patients who have decisional capacity at the time of formulating an anticipatory plan, and Best Interests Decision making, for individuals who lack ‘decisional capacity’ and therefore cannot make informed choices regarding health and social care needs.
Since then, conference organisers have been collating, analysing and evaluating the copious data from this national conference, to establish how it can best inform, the future care planning priorities for Wales, prudent healthcare and the value based healthcare approach. In parallel, the Advance & Future Care Planning Strategy Group for Wales is undertaking a more detailed evaluation to recommend and recommend documents for practical use in day-to-day future care planning. Current findings have identified the need for single document approach for Wales, using the NHS Wales logo and ensuring ease of recognition, communication and transferability. Here, we provide a summary evaluation of conference data, to outline how comments and agreed key points from participants have been categorised into themes.

Background:
This strategic approach sets out a vision for Advance and Future Care Planning in Wales. It has clear links to key policy documents such as to ‘Prosperity for All’ [2] and a ‘Healthier Wales’[3] and aligns with many of the principles set out in the ‘Future Generations Act’ [4] and the Prudent Healthcare approach [5]. In April 2016, the Well-Being of Future Generations Wales Act came into effect and we see the Act as an opportunity to ensure our services are not only fit for the future but that everything is framed for the long term, considering prevention, integration, collaboration and involvement. The Act’s 7 Well-Being goals and 5 ways of working align with Advance and Future Care Planning Goals and will form part of the ongoing approach, for instance with setting up a central national electronic patient record repository.
Methods:
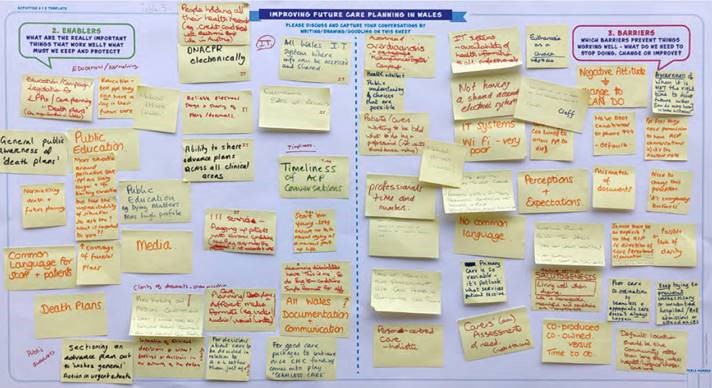
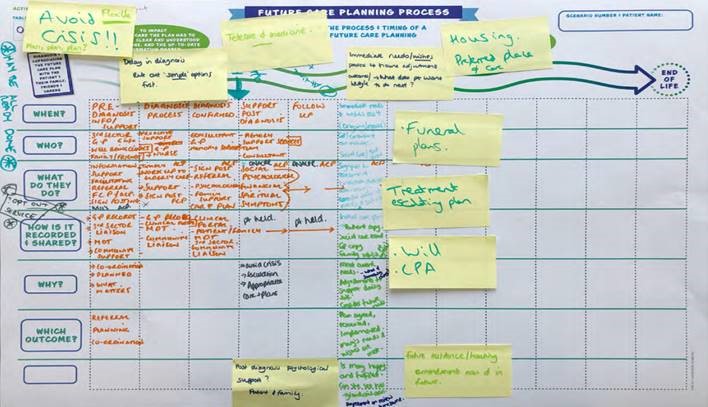
Data from four sequential activities in which all conference attendees participated have been transcribed and collated. Activity 1 was in essence an ‘icebreaker’ to encourage attendees to share knowledge regarding FCP. Activities 2 and 3 captured attendees understanding of on-going ‘barriers’ and ‘enablers’ to FCP (pic 1) illustrates key areas agreed upon, and written down as summary statements from one workshop group. Activity 4 (pic 2) required attendees to annotate a detailed outline of designing a patient future care plan and the ‘journey’ involved for different scenarios (each table had different situations and challenges to ponder). All the data from the four delegate activities was generated by multi-professional attendees, patient advocates and representatives, hence a co-productive process involving all geographical areas of Wales. Following data transcription and collation a meeting was held at the Marie Curie Research Centre in Cardiff, to agree on data analysis in terms of emerging themes, how these are best categorised to inform the next stages of an ‘All Wales FCP document and process’.
Results:
Key outputs from the conference per se, included acknowledgement that the FCP documents produced will need to be easy to identify (e.g. paramedics or Out of Hours GPs often need to quickly locate FCP documents to inform time-critical decisions), interpret and also update, whilst being specific and detailed enough to impact clinical decision making.
Themes within the barriers activity included people’s perceptions and sometimes misconceptions of the process of Advance Care Planning, time constraints and inability to easily share outcomes, for instance via electronic patient records across all provider services and care settings. The lack of an agreed ‘language’ to describe FCP in terms of both its process and the on-going documentation, for example when paramedics enter a patient’s home there is no agreed term for them to easily ask patients/ relatives for FCP documents.
A major theme in workshops and written feedback from this conference was an awareness of the weaknesses of the generic term ‘advance care planning’. Participants found that even healthcare professionals would not always understand the term, and there would frequently be confusion between advanced and advance, with some professionals and patients believing it referred to enhanced care, rather than prior/anticipatory planning (Advanced = better, advance= prior). A general consensus, voiced by patient/carer representatives at this conference, was that the term future care planning left less doubt in their mind that this was a process that involved talking about future scenarios/crossroads, and writing down what views patients might have on the different options that may be on offer at such a timepoint. One participant commented that the recent international white paper by the European Association for Palliative Care, which sets out a definition of advance care planning, means that as a process it only applies to patients with capacity from the outset. So it is excluding of those patients with diminished or fluctuating capacity. The newer term Future Care Planning therefore offered an opportunity to offer all the benefits of ACP to patients and those lose to them where capacity was not present at the time of holding these discussions and/or making important decisions. A best interests approach to find out what the individual would have wanted, given a specific set of circumstances, and asking those lose to the patient how they (the patient) might have responded, if a feeding tube, for instance, were offered, was felt to be a vital part of the future Care Planning processes and offerings.
Key ‘enabler’ themes were identified as education, both public and professional; patient involvement and an ability to have an all Wales approach similar to the national DNACPR policy. Participants in the Future Care Planning process exercise considered all important areas of life that this might impact, including preferences for place of care, housing, place(s) of death (patients want flexible options, not just one preferred place of death).
Conference delegates also reflected, discussed and agreed on the FCP process in terms of who should be involved and how data is both recorded and shared. Concerns were heard about challenges in sharing established wishes, decisions or refusals of treatment when these had been made, but were not reaching all parts of the health and social care service. Concerns were also voiced about paper format, photocopies of DNACPR forms, version control (a form has been written but patient has then asked for it to be changed or scrapped). Enablers to better sharing needs to be found via a central electronic patient repository, with an ability for all health and social care services to access this data.
Conclusion:
Data from the conference and input from patient representatives have fed into the development of a detailed specification document identifying what an electronic patient record holding Future Care Plans should look like. What it should include and how it should be shared. This has been one of the key outputs of the national Advance and Future Care Plan Strategy Group for Wales, chaired by Mark Taubert.
There has been on-going teaching on the Serious Illness Conversation Cymru programme [6] and Future Care Planning education sessions to the Welsh Renal Network (Cardiff, Swansea and Wrexham). Teaching for Paramedics to facilitate interpretation of Advance Care Planning and Future Care Planning documents continues. All current FCP education includes the ‘Message in a bottle’ scheme, where details of ACP/FCP forms are kept in a bottle in the fridge for healthcare professionals to find in a person’s home. However as Dr Taubert stated at the close of FCP conference (2019), shared electronic patient records that enable direct input from patients must be the future: “Shared Decision making should also include an ability to share the decisions that have been agreed on”, he said.
Last but not least, a database has been initiated at conference, which requested attendees put themselves, or colleagues forward for the next stage of FCP strategic planning for Wales. This will involve a ‘task and finish’ group that will take forward the Framework Analysis output. Whilst much work needs to be done, it feels we have now taken significant steps in creating a consensus approach in this important area.
References:
[1] Rietjens J, et al Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care, The Lancet Oncology,Volume 18, Issue 9,2017, pp e543-e551,ISSN 1470-2045, https://doi.org/10.1016/S1470-2045(17)30582-X.
[2] Prosperity for All: economic action plan. Wales: Welsh Government; Welsh Government (2018)
[3] A Healthier Wales: our Plan for Health and Social Care. Wales: Welsh Government;Welsh Government (2015)
[4] Well-being of Future Generations (Wales) Act 2015. Wales: Welsh Government
[5] Simply Prudent Healthcare – achieving better care and value for money in Wales – discussion paper. Wales: Bevan
[6] Pease NJ, Sundararaj JJ, O’Brian E, et al Paramedics and serious illness: communication training