Co-speciality supportive care pathways running in parallel with ‘standard’ care? A sustainable, effective and highly rated model of care for patients with advanced heart failure which has potential transferability to other non-cancer advanced stage conditions.
by Dr Clea Atkinson, Consultant in Palliative Medicine and Bevan Commission Fellow, Velindre University NHS Trust and Cardiff and Vale University Health Board,
Professor Zaheer Yousef Consultant Cardiologist and Heart Failure Specialist, Cardiff and Vale University Health Board (C&V UHB),
Sian Hughes Specialist Palliative Care Nurse, University Hospital of Wales, Cardiff, Wales, UK

Introduction:
In early 2016, a Heart Failure Supportive Care pathway was initiated in Cardiff and Vale University Health Board (C and V UHB), as a means to improve the experience of patients with advanced heart failure in the last years of life. It is well recognised that these patients have a poor quality of life and a high symptom burden; often equivalent to patients with metastatic cancer (1).
The expanding non-cancer remit of palliative care has provided an ideal opportunity to explore ways to address the holistic needs of this vulnerable group of patients. However, although there are some published service designs with improved outcomes, there is no consensus as to the best approach for addressing the needs of these patients or clear thinking on which models of care may be able to offer cost improvements, whilst concurrently providing a good patient experience (2).
Dr Clea Atkinson is clinical lead for the project, working collaboratively with Cardiologist Professor Zaheer Yousef, Sian Hughes Specialist Palliative Care nurse and the Cardiff and Vale UHB Heart Failure team.
An initial scoping exercise and literature review identified several areas in need of development including:
1. Effective communication with patients and carers to improve understanding and acceptance of the limits of prognosis (many patients have received highly invasive and technical treatments and struggle to transition to a more non-invasive/supportive management strategy).
2. Palliation of high symptom burden (local data has demonstrated a pattern of disabling symptoms experienced by this patient group which are often unrecognised).
3. To discuss and implement patient’s advance care planning choices (recognising that this needs to be a compassion based process which occurs at a patient’s own pace).
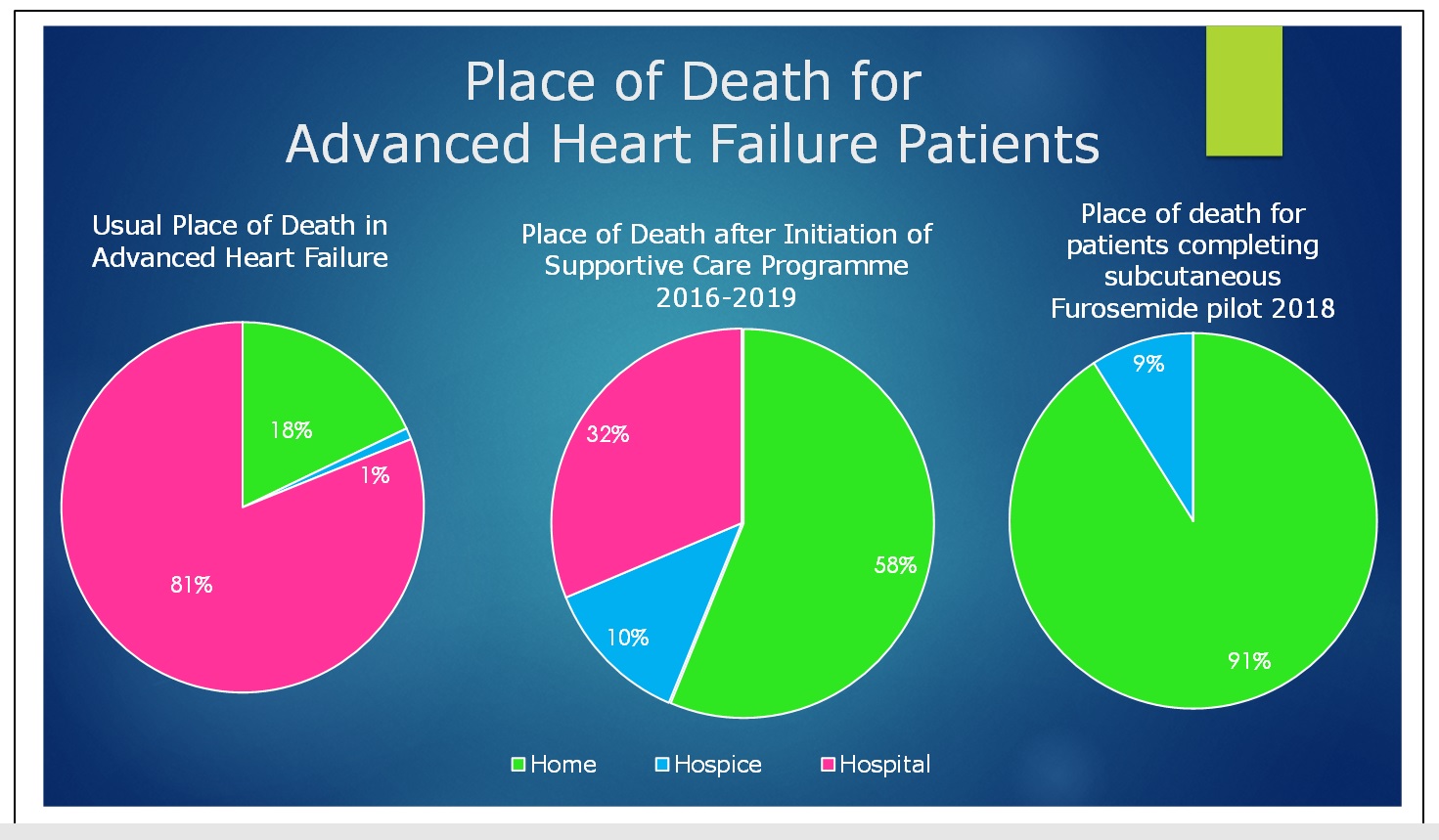
4. To respect patient’s choices regarding enabling end of life care to be in their preferred place of death (around 80% of HF patients who would choose to die at home, currently die in hospital).
Service model:
The Cardiff Heart Failure Supportive Care Team (HF-SC) consists of a palliative care consultant, consultant cardiologist and specialist palliative care & heart failure nurses who now meet on a weekly basis through multi-disciplinary team (MDT) meetings and joint clinics (hospital and community-based locations) which has facilitated a truly transitional model of care.
The referral criteria aims to capture patients with advanced heart failure in the last 1-2 years of their lives and this pathway encourages much earlier referral supported by the governance step of discussion at a multi-disciplinary meeting (Pic 1), ensuring that patients are referred after expert review has confirmed that all appropriate active management has been optimised.
Inter-speciality updates and dialogue at the regular multidisciplinary team meeting:
The initial focus for palliative care has been building rapport and improving symptom control, this being central to gaining trust of these patients who generally have great faith in their referring team. This is core to changing every patient’s experience which otherwise becomes increasingly led by fear and subsequent dependency on acute services. Providing holistic assessment and building strong compassion-based relationships with patients and carers allows each individual’s perceptions, experience and what matters to them most to be heard and understood, underpinning an effective process of supportive management including advance care planning.
Co-speciality joint clinics (Pic 2) are an important and innovative aspect of this service where patients are reviewed by both cardiology and palliative care specialists together, with the benefit of both disciplines providing their expertise simultaneously. This clinic gives opportunity for patients to be directly referred person to person between specialities, which not only supports transitioning but also fosters ongoing rapport whilst providing tailored management for each individual and therefore balancing the greatest possible survival benefit with maximal focus on quality of life.
Co-speciality cardiology and palliative care clinic with joint patient review:
A transitional model of patient care has enabled the referring speciality to have more confidence in making earlier referral because exact prognostication is not so necessary and the cardiology team can continue their involvement with patients whom they have often known for a very long time and their involvement can continue by providing ongoing joint expertise with inter-speciality dialogue allowing discussion and joint decision-making.
“It is absolutely crucial to have an end-of-life service that complements the intensity and quality of the complex interventions and care invested in our heart failure patients. Our patients are very fortunate to now have access to such a service.” – Professor Zaheer Yousef
Emphasis on building respectful relationships between specialities whilst listening to and working together with patients has allowed hugely valuable co-production, development and delivery of this Supportive Care service and is allowing shared expertise and mutual learning to drive further improvement.
The cross-boundary approach allows management to be more joined-up across various settings in response to the individual patient journey, improving co-ordination between healthcare providers and allowing continuity as a key way to ease patient fear. The referring team are frequently updated and can still offer clinical input to the patient in all settings by linking with the primary care teams, community and supportive care teams even as the patient gradually moves towards a more palliative approach.
The introduction of subcutaneous furosemide infusions in the community as a means of managing episodes of fluid overload in patient homes has been a further valuable element of this model. Patients are selected if they are being acutely admitted for what is effectively palliation with IV Furosemide or who are requesting not to be admitted to hospital again. A bespoke treatment plan is ready in the home which can be used when a patient’s condition worsens in an anticipated and proactive way, which is avoiding repeated hospital admissions and maximising time in preferred place of care and so more often achieving preferred place of death. District nursing involvement in delivering care can then facilitate moving into the end of life phase more readily when this is needed.
In order to support the desired outcomes of advance care planning which are often difficult to achieve this is integrated into the pathway as an ongoing process with each patient moving at their own pace and then using the cross-boundary model to support their wishes to happen wherever they may be.
Key Achievements and Outcomes:
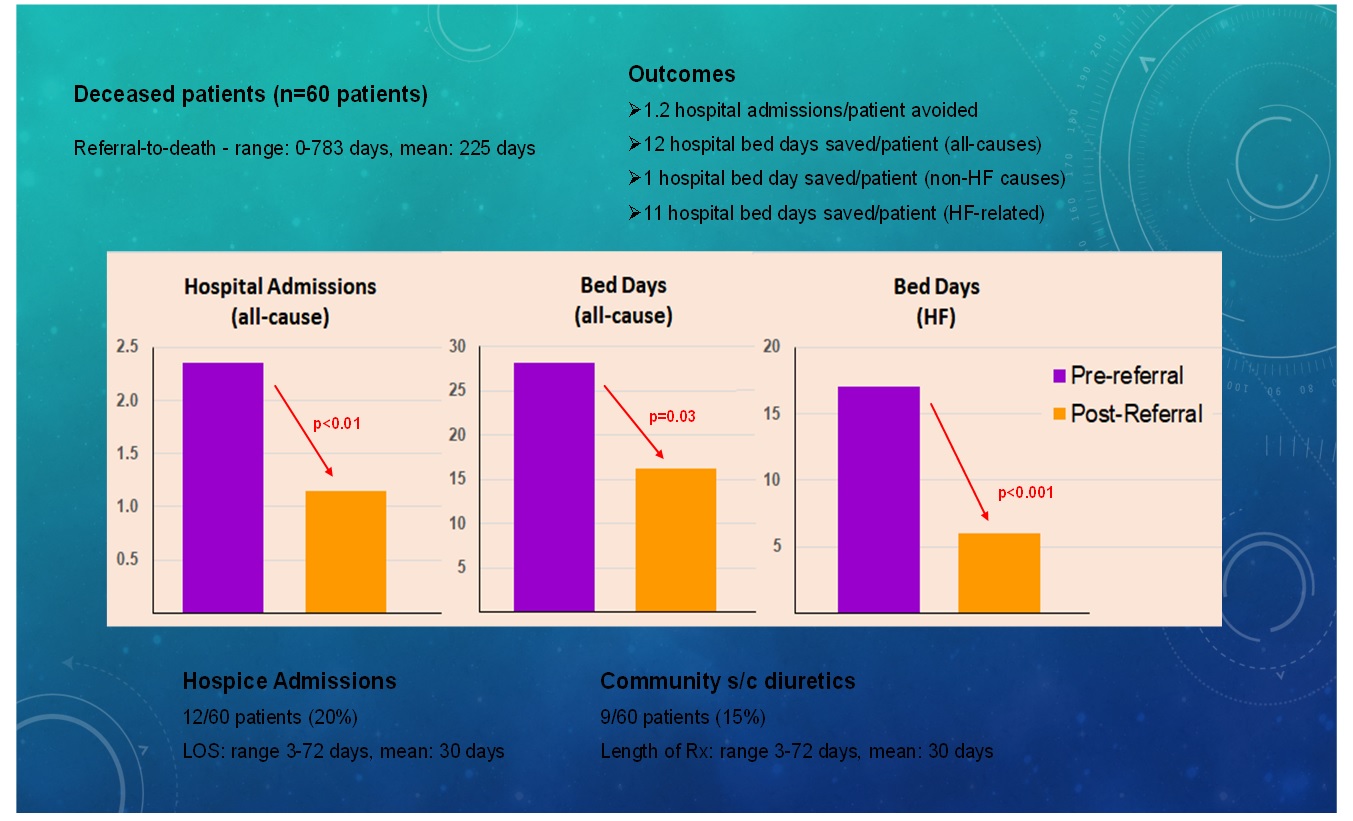
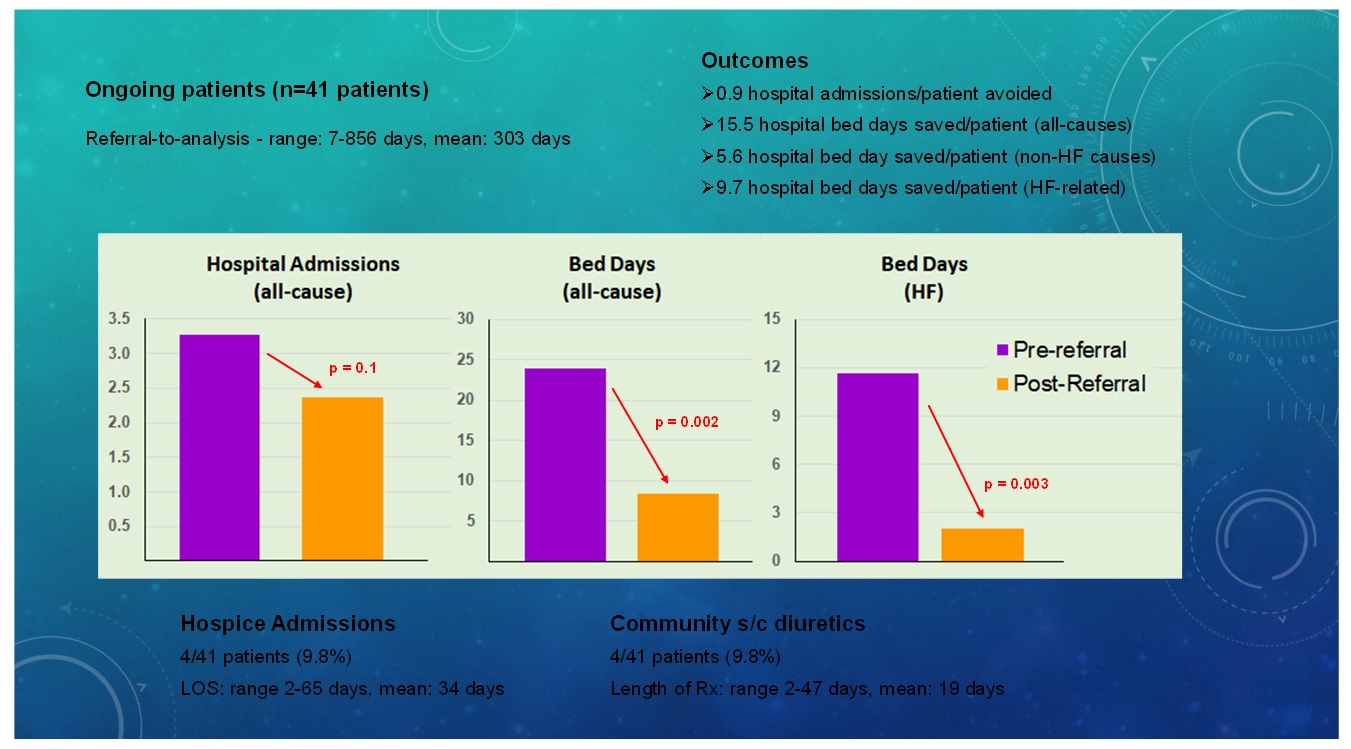
Evaluation of the first 3 years of the project has included 101 patients referred to our service; 60 patients are now deceased (mean time in service: 225 days), and 41 are still receiving on-going care (mean time in service: 303 days). We compared a period of a year prior to the point of referral with the time after referral until death or up to the time of the service evaluation (Pic 3).
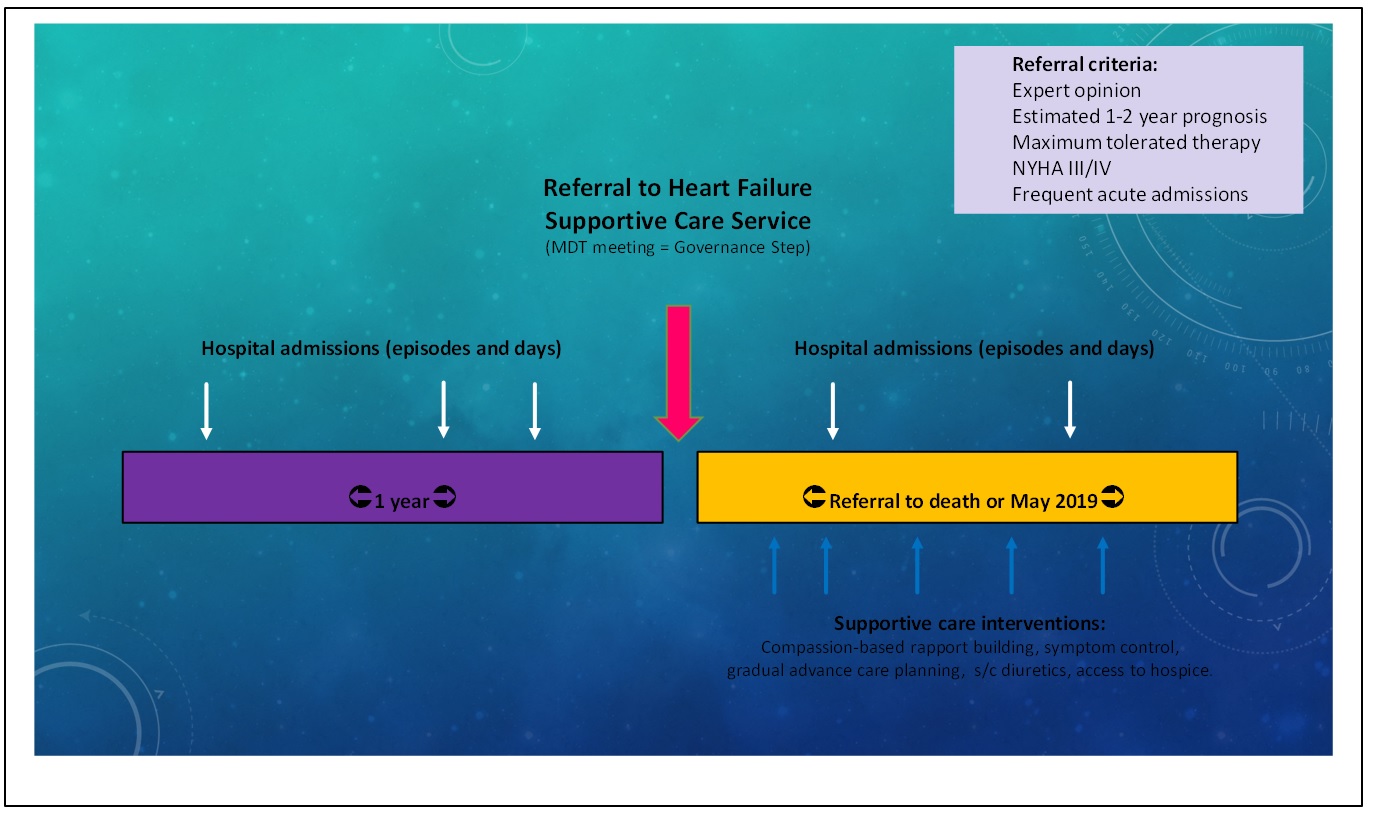
The time under the service is increasing for the ongoing patients compared with those who have already died, reflecting the evolution and maturation of the pathway over the past 3 years. Overall 12 hospital bed days were avoided for each deceased patient and 15.5 bed days for each on-going patient so far. The greatest reduction has been with heart failure related admissions, reflecting the fact that patients are still able to be admitted to acute services if necessary and appropriate (Pic 4, 5). The overall referral rate for cardiac patients to palliative services has tripled.
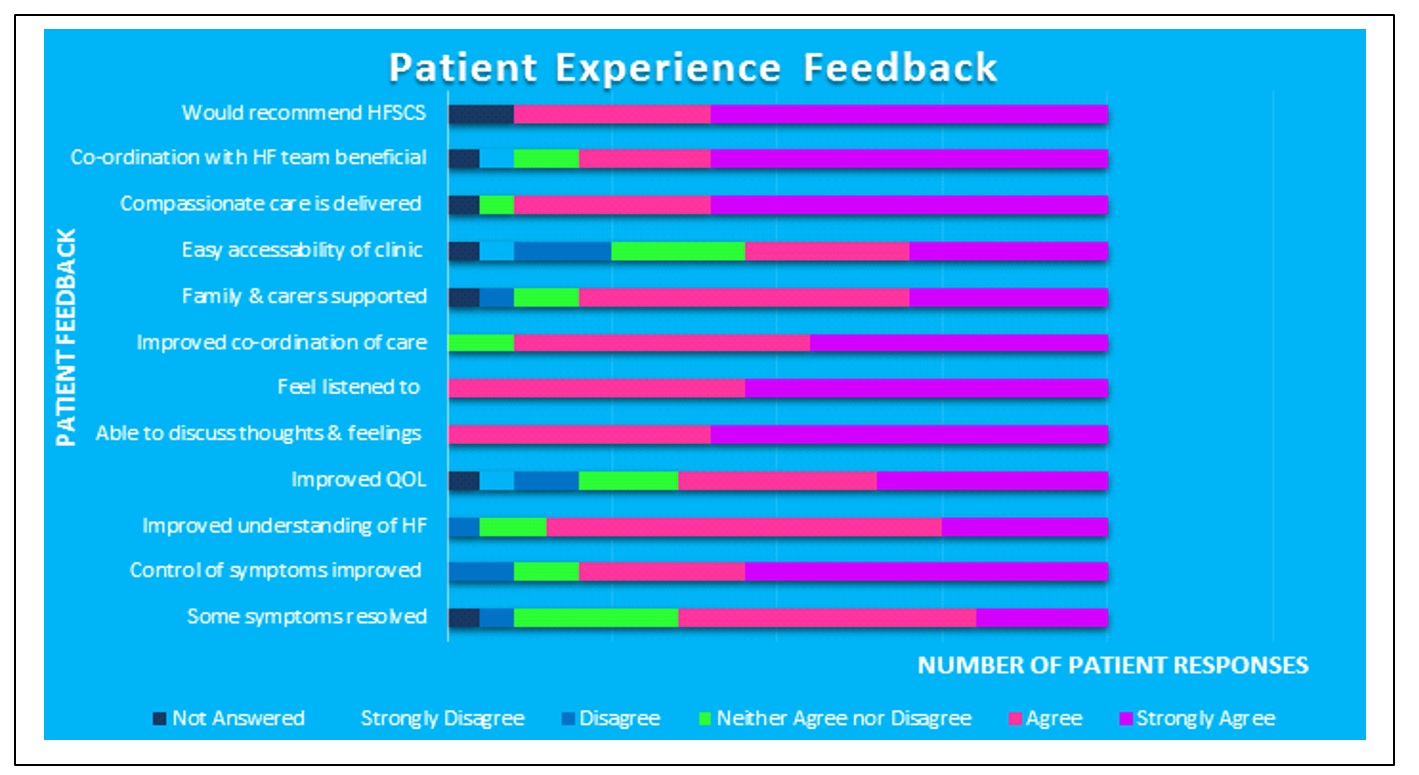
A snapshot review of all patients alive and under the service at one point in time was carried out and patient experience of 25 patients was evaluated by postal questionnaire. An exceptionally high 80% response rate was achieved on first return. 100% of patients said they felt listened to and that they could discuss their thoughts and feelings. 90% of patients responded that they would recommend the service to others and that the care they received was compassionate and coordinated.
80% of patients surveyed reported that symptom control was improved, found the service supportive for carers and that integration of care with the cardiology heart failure team was beneficial. (Pic 6, patient consent for image sharing obtained). Representing carers, Mrs Peta Williams, the wife of David Williams, a patient under the Supportive Care service who died peacefully at home as he had wished, commented: “This is the NHS at its best.”
Death at home (preferred place of death) has increased from 18% to 58% and death in hospital has reduced from 81% to 32%. Preferred place of death was achieved in 100% of patients in the 12 month s/c Furosemide pilot. (Pic 7).
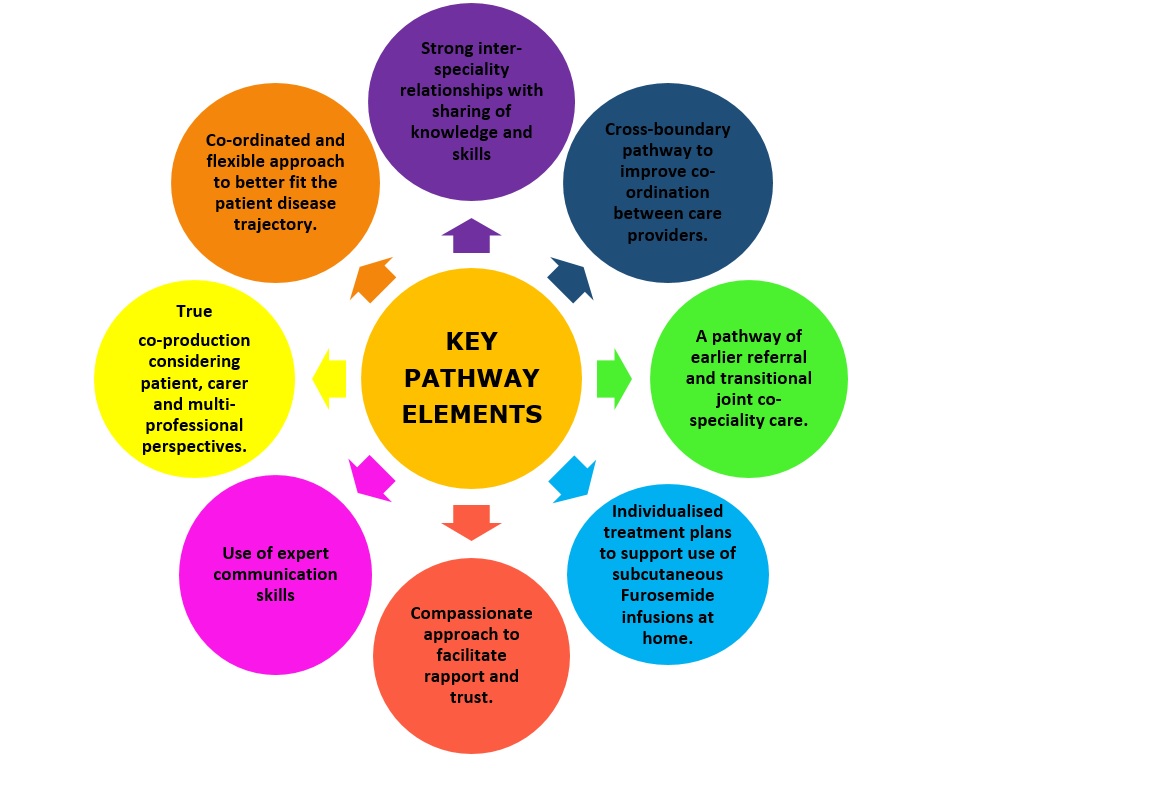
We strongly believe that there is a more than add-on value of bringing together all key elements (Pic 8) of this model which has created the superior success and effectiveness of this pathway. This continues to be refined using a transformational change strategy.
Key pathway elements:
Financial benefit: The overall cost-savings of the supportive care element are considerable. Unwanted/unwarranted hospital admissions, hospital bed days saved, when calculated, can equate to £8000-10000 per year, per patient, or around £3million per year for the population of Cardiff, when extrapolated.
The Future Potential
Financial support from both the Heart Disease Implementation Group (HDIG) and the End of Life Board in Wales facilitated the first phases of this project. The value of this approach has now been recognised by the Cardiff and Vale UHB ‘Spread and Scale Academy’ who are supporting Dr Clea Atkinson in this work. She has also been awarded a two year Fellowship by the Bevan Commission in Wales to provide support to other local Health Boards who wish to adopt similar models of care for their advanced heart failure patients.
Furthermore there is considerable interest regarding the transferability of the key elements of this model of care in other life-limiting conditions such as COPD, pulmonary fibrosis, advanced stage renal failure, adult congenital heart disease and advanced stage liver disease by adoption of the key elements of the pathway. Specific anticipatory treatment plans for the most likely causes for repeat admissions in these different clinical situations in their advanced stages are being evaluated.
References:
1. Bekelman et al (2009). Symptom burden, depression and spiritual well-being: a comparison of heart failure and advanced cancer patients. J Gen Intern Med;24(5):592-8
2. Johnson M.J, McSkimming P, McConnachie A, Geue C, Millerick Y, Briggs A, Hogg K (2018). The feasibility of a randomised control to compare the cost-effectiveness of palliative cardiology or usual care in people with advanced heart failure: Two exploratory prospective cohorts. Pall Med; 32(6): 1133-41.