Blog by G. L. Krishna
A recent notification in The Gazette of India: Extraordinary1 has formalised the initiative of the National Commission for Indian System of Medicine to start Doctorate of Medicine (DM) courses in ayurveda. DM courses will be introduced for six subjects: psychiatry, hepatology, oncology, orthopaedics, reproductive medicine and gerontology. They are “intended to produce super specialists with deep understanding in ayurveda classics with updated knowledge in contemporary sciences in the relevant speciality areas.” This step appears temerarious because traditional medical systems like ayurveda can claim no major role in speciality and super speciality areas.
Traditionally, DM courses are meant to train medical postgraduates in super speciality areas. While a graduate degree equips a physician to function at the level of primary care as a general practitioner, postgraduate medical study is meant to create specialists who deliver secondary care. Programmes such as DM, which usually select only specialists for training, aim to create doctors with a deeper expertise in a particular subspeciality.
Ayurveda is an ancient science that developed when the methods of collecting and evaluating evidence were nascent. Its understanding of life-processes in health and illness was sketchy and often conjectural. However, its observations on health-promotion and illness-management, reinforced by the documented experiences of physicians across centuries, retain validity; but this validity comes with caveats. The foremost caveat is this: given that traditional medical systems are backed only by soft evidence, it is imprudent to use their prescriptions as stand-alone treatments in high-risk clinical situations.
To illustrate, mild depression is a common presentation in primary care settings. It can be addressed safely and effectively with the interventions of ayurveda and yoga. Ayurveda’s emphasis on holism and the gentleness of its approach, as well as its cultural acceptability, make it especially relevant in managing such cases in the context of the psychosocial stressors underlying them. The option of referring to higher levels of care if the condition does not improve is always open. But severe depression with psychotic symptoms and suicidal risk usually requires an urgent referral to specialists trained in psychiatry. Ayurveda and yoga are good to use only as complementary systems in the management of severe cases; they cannot serve as alternatives to conventional management.
By and large, traditional medical systems are usable in primary care when employed after careful safety netting and with scientific prudence. As the Oxford Textbook of Medicine explains, “When it is of proven quality, safety and efficacy, traditional medicine contributes to the goal of ensuring that all people have access to care that they feel they need.”2 Even in primary care, cases that need acute management are best left to modern medicine.
Ayurveda’s sketchy understanding of life-processes, its diagnoses based on ancient heuristics, and the soft evidence that backs its prescriptions are features that diminish its role in speciality areas. Merely supplementing ayurvedic texts with current science will not rectify these lacunae. While current sciences certainly help in making a more prudent use of ancient knowledge, they cannot artificially stretch its scope. Conceiving a super speciality DM Hepatology course based on a system that had only a vague understanding of liver functions and pathologies is a result of policy-makers’ misdirected zeal. Likewise misdirected are plans to start a DM Oncology course based on ancient texts that had not the remotest idea of cancer as a generic pathology. Parity between systems does not come by merely mimicking the academic hierarchy of modern medicine. Medicine is not mimicry.
Researchable propositions in speciality areas may certainly be gleaned from the ayurvedic classics, but a researchable proposition does not ipso facto become an employable clinical guideline. It is the mandate of the Central Council for Research in Ayurvedic Sciences (CCRAS) and its numerous regional centres to look into ayurveda’s researchable areas. Super speciality courses in under-researched areas cannot justifiably usurp that mandate.
Such a usurpation would have two undesirable consequences. First, it would misinform the public, suggesting that ayurveda has a major role in the management of serious pathologies like cancer. Misinformation of this sort would only lend credence to the overblown claims that charlatans make time and again. It may be recalled that the Supreme Court of India has recently come down heavily on an ayurvedic drug company for its misleading claims. Second, ayurveda, which has always insisted that its physicians be humble and truthful in their claims, would become subject to further caricaturing by its vociferous distorters.
The Charaka Samhita showed contempt for fraudulent physicians and warned, “Fraudulent physicians blow their own trumpet and move from place to place in search of victims. They seldom ask or entertain questions. They are the envoys of death.”3 In its temerarious zeal to promote ayurveda, may the National Commission for Indian System of Medicine not end up becoming an unwitting supporter of the type of fraudulent physicians whom Charaka despised.
G. L. Krishna is an ayurveda physician. He is also a research scholar at the National Centre for Biological Sciences – Tata Institute of Fundamental Research, Bengaluru, India. He may be contacted at krishnagl@ncbs.res.in. He welcomes comments from readers via email.
Notes
[1] The notification was published on October 4, 2024 and can be accessed The Gazette of India’s website by searching with the gazette id CG-DL-E-07102024-257729.
[2] Fulong Liao et al., “Traditional Medicine Exemplified by Traditional Chinese Medicine,” in Oxford Textbook of Medicine, 6th edition, ed. John Firth et al. (Oxford University Press, 2020) 108. https://doi.org/10.1093/med/9780198746690.003.0014.
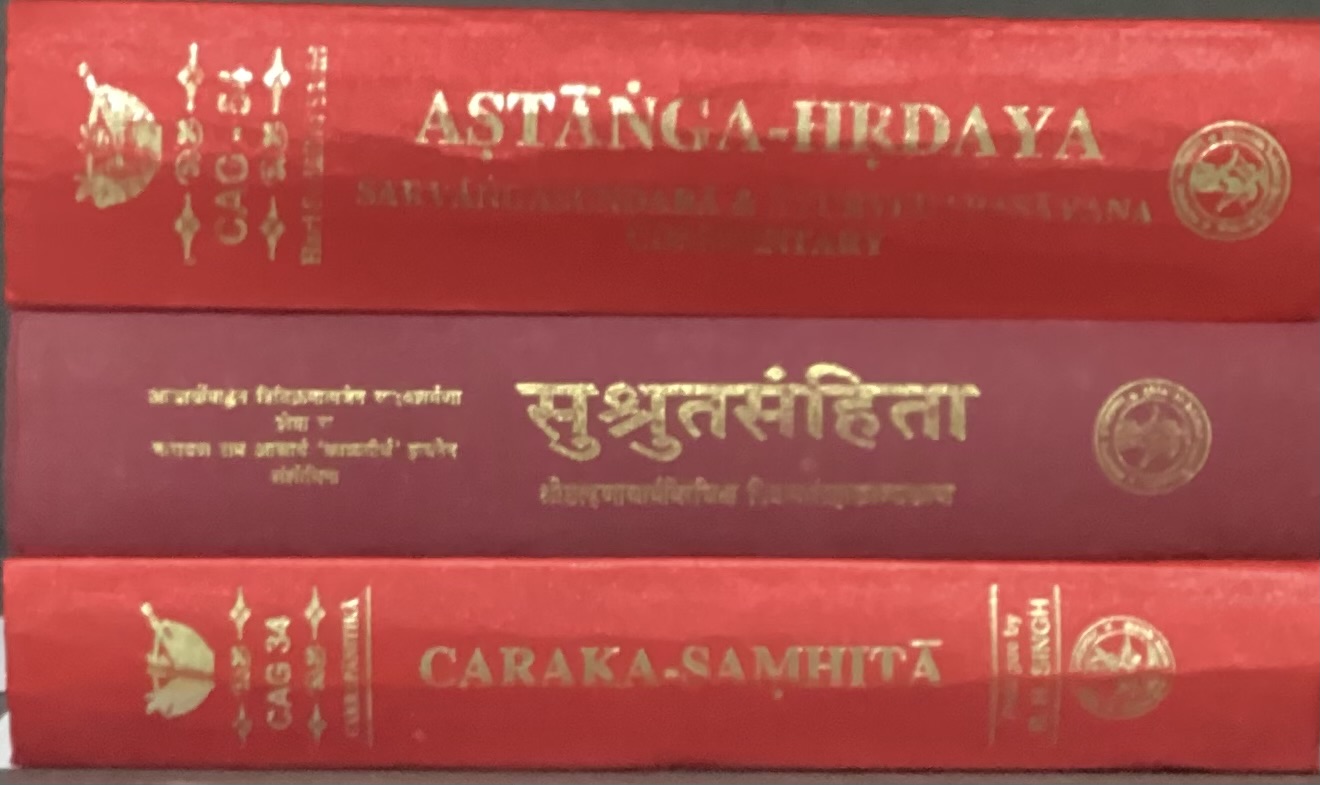
[3] Charaka Samhita (representing the school of medicine) and Sushruta Samhita (representing the school of surgery) are the two classics on which ayurveda is based. The Samhitas bear the names of their authors/revisers, and their earliest versions date back to the first millennium BCE. The present quotation is taken from the twenty-ninth chapter of the section called Sutrasthanam in Charaka Samhita.