Checkpoint inhibitor drugs are a relatively new immunotherapy for cancer, showing outstanding clinical efficacy in various tumors, including lung cancer and melanoma. By improving the immune response to disease, these drugs also trigger immune-mediated side effects, which can compromise the nervous system. Among all the neurological complications, the peripheral nervous system (PNS) is commonly affected by neuropathy, myasthenia gravis, and myositis. However, central nervous system (CNS) complications by immune checkpoint inhibitors (ICIs) are less characterized, and knowledge regarding clinical, imaging, and treatment responses are scarce.
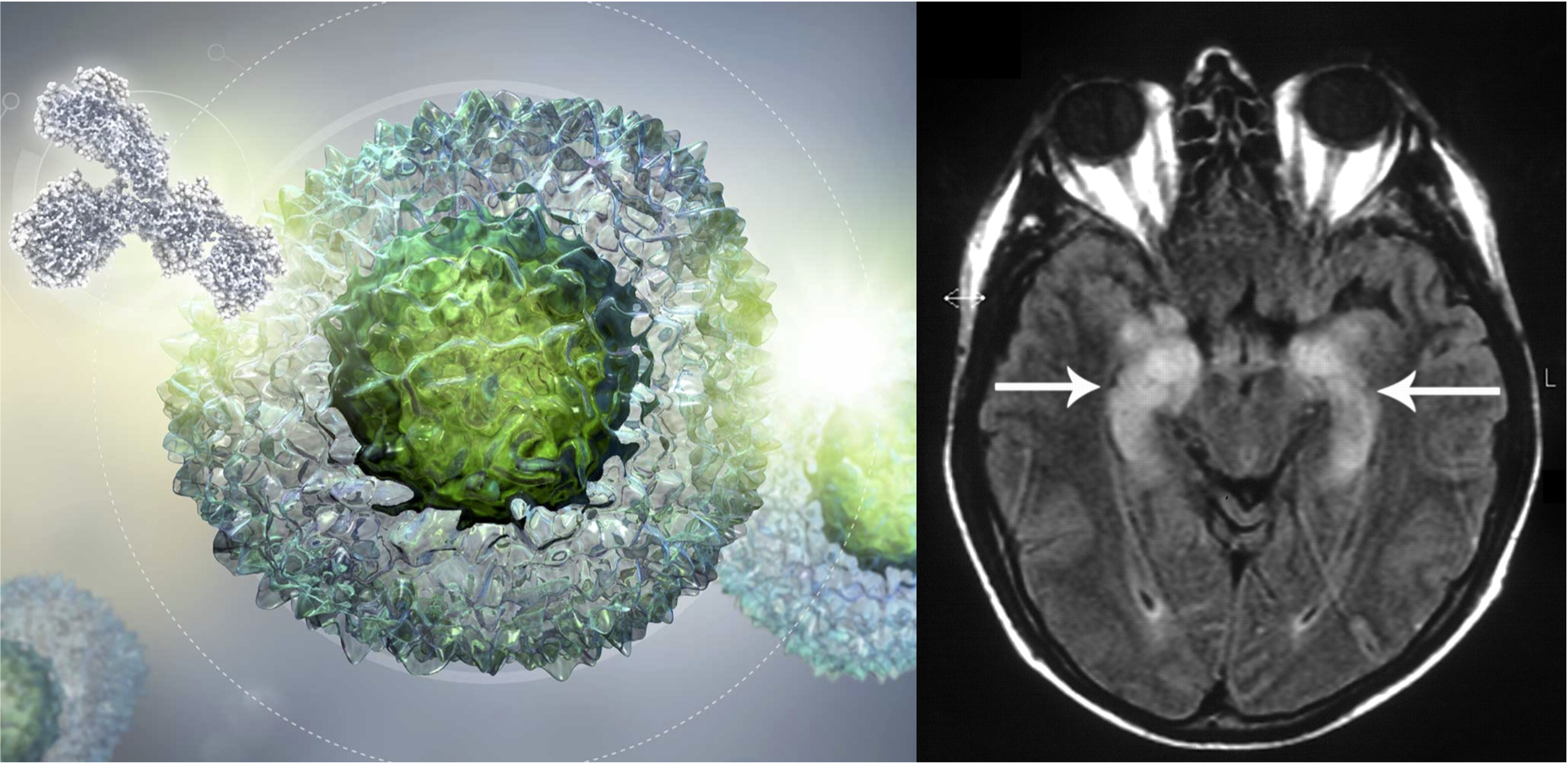
In the July issue of JNNP, Vogrig and colleagues describe the largest cohort of patients with CNS complications secondary to ICIs (Figure 1). Retrospectively, patients were selected from the French National Reference Center for Paraneoplastic Neurological Syndromes and Autoimmune Encephalitis (Lyon, France) and clinical and ancillary data were extracted. A total of 19 patients were identified, of whom 8 patients presented with limbic encephalitis, 4 with meningoencephalitis and 4 with cerebellitis. Two patients developed isolated confusion and one parkinsonism. Regarding autoantibody studies the most commonly detected were onconeural antibodies, followed by astrocytic and neuronal surface antibodies. As part of the treatment, in all patients ICIs were withdrawn and corticosteroids were used. Another treatment used was IVIG, rituximab, plasmapheresis and infliximab. The series mortality was 32% (6 cases). When the authors compared patients with CNS dysfunction versus PNS dysfunction triggered by ICIs, the former had significantly more frequent non-small-cell lung cancer (NSCLC; p<0.01) and positive autoantibodies (p<0.01) than patients with PNS dysfunction. There was a trend towards a poorer outcome in the CNS group.
ICIs have become standard treatments for many cancers; therefore, neurologists should be aware of the immune-related adverse events associated with this new drug group. In this JNNP article three main clinical phenotypes (limbic encephalitis, meningoencephalitis and cerebellitis) were fully characterized to understand the clinical picture and outcome of CNS dysfunction secondary to ICIs. Of interest, this group of patients frequently have NSCLC, positive autoantibodies and worse outcome. Given the lack of biomarkers for diagnosis, it is crucial not to forget to exclude a wide range of disorders including infectious, metabolic, endocrine or metastatic diseases in this group of patients. Further studies are needed to understand the immunopathogenesis, define specific treatment approaches, and identify patients with cancer who are at risk of developing CNS dysfunction triggered by ICIs.
Read more at https://jnnp.bmj.com/content/91/7/772