Functional neurological disorders are increasingly prevalent, but a limited understanding of their pathophysiology continues to make this one of the most challenging disorders seen in neurological practice. Its chequered history is reflected in outdated terms such as ‘hysteria’, ‘psychogenic’ and ‘non-organic’, and for the present time, the term ‘functional’ has been adopted for use in clinical practice. The social and health economic impact is substantial, largely due to loss of work and dependence on illness-related benefits. In this cumulative way, it has commonly been described as “a crisis for neurology”.
The paper by Wissel et al published in the latest edition of JNNP explores functional neurological features in patients with Parkinson disease (PD-FND), retrospectively reviewed across multi-centre sites from electronic records. 34% of patients were found to have functional symptoms at the time of their PD diagnosis, with a predominantly female representation (68%) and a pre-morbid profile of pre-existing psychiatric disorders and a family history of PD. Functional tremor (FT) and gait impairment were found to be the most common phenotype (40%), in keeping with current literature suggesting that the former is the most common presentation of functional movement disorders overall.
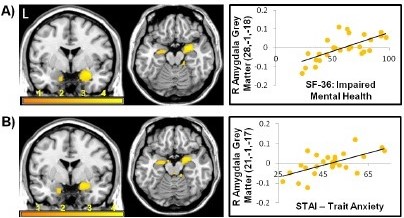
Figure 1: mental health and anxiety correlates with increased right amygdala volumes in functional neurological disorders. (A) Impaired mental health and (B) Anxiety (Perez et al, JNNP 2017; 88:1052-1059).
Interestingly, the authors also found that psychiatric features were disproportionately greater in the PD-FND cohort than overall motor disability, with a relatively increased severity of depression/anxiety. This deserves some separate consideration. Although traditional definitions of functional neurology emphasised psychological causation, this association has recently been questioned. Indeed, the frequent presence of coexistent psychological disturbance in organic PD makes such symptoms hard to differentiate, as indicated in the article. However, recent findings of abnormalities in the amygdala (figure 1) and supplementary motor area (SMA) may justify this demonstrated over-representation of psychological symptoms in PD-FND. Specifically, one hypothesis connecting these regions is that such patients may be sensitised to emotionally arousing events, triggering functional movement controlled by the SMA (disconnected from control by the prefrontal cortex). Clinically, this may therefore translate to an increase in psychiatric symptoms in this cohort, in-part explaining the authors findings. This encourages further consideration of the biopsychosocial models of PD-FND and across the spectrum of functional neurology, and exposes some of the complexities of the clinical disorder in PD-FND. Overall, Wissel and colleagues have raised important concepts regarding the overlap of organic and functional phenomenology, highlighting the need to be alert to this in clinical practice.