In the November issue of JNNP, Meoni and colleagues have published an interesting observational retrospective study exploring the long-term effect of pallidal deep brain stimulation (DBS) on motor and functional disability in patients with idiopathic, inherited and acquired dystonia. DBS is a neuromodulatory strategy base on a brain implanted electronic device used to modulate the neuronal functioning in a particular brain region or network. DBS of the globus pallidus internus (Gpi) has been demonstrated to be an effective treatment that improves motor symptoms and disability in patients with idiopathic and inherited dystonia. However, DBS has been suggested to be less effective in acquired dystonia. Until now, the long-term efficacy and safety of DBS in patients with idiopathic, inherited and acquired dystonia have not been previously established.
The authors studied a cohort of sixty-one patients with medication-refractory dystonia who were absent of active severe psychiatric symptoms or medical contraindications for surgery. Patients included were videotaped and assessed preoperatively and postoperatively (follow-up 7.9 ± 5.9 years) using the Burke-Fahn-Marsden Dystonia Rating Scale, which includes motor and functional disability scores. Patients with idiopathic and inherited isolated dystonia presented a significant improvement of motor symptoms at 1 year (58% improvement of motor score), which was maintained at the last follow up (57%). Patients with acquired dystonia only had modest motor improvement, which remained stable over time. Regarding disability scores, patients with idiopathic and inherited isolated dystonia presented with a significant improvement both at 1 year (37.4%) and at the last follow-up (23.3%), in comparison with assessment before DBS implantation. Interestingly, there was a trend to lose this improvement over time. Patients with acquired dystonia also had significant improvement in the disability score at 1 year follow-up (23.4%), but lost this effect over time. Finally, seven patients (11.4%) had surgery related complications and fourteen patients (22.9%) presented stimulation induce dysarthria. There were no permanent neurological deficits in patients who presented with adverse events.
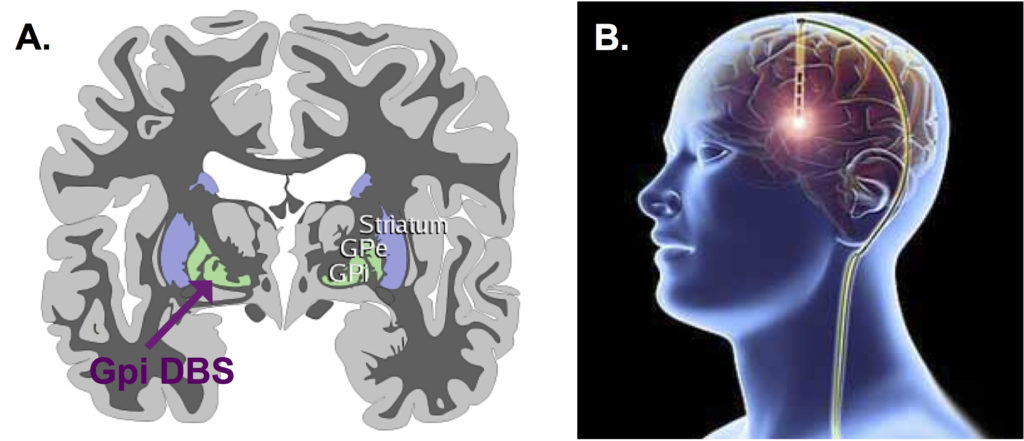
DBS has been increasingly used in a variety of movement disorders since its introduction into the therapeutic armamentarium in the 90s, and its use has been particularly represented in essential tremor, Parkinson´s disease, and dystonia. Even though its precise mechanism of action is not fully understood, its effects on local excitatory and inhibitory circuits, together with brain network modulations, results in significant symptomatic improvement in these movement disorders. The present study demonstrates that pallidal DBS is an effective and safe treatment for dystonia and has confirmed the poorer long-term outcome in patients with acquired dystonia in keeping with previous studies. Further studies are now required to carefully define prognostic factors and improve patient selection.
Read more at http://jnnp.bmj.com/content/88/11/960