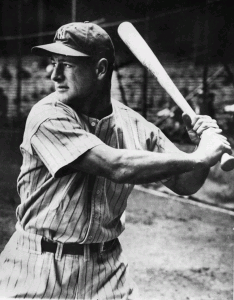
- Lou Gehrig “Gibraltar in cleats” In the midpoint of the 1938 season, it became clear there was a problem. James Kahn, a reporter who wrote often about Gehrig, noted in one article: “I think there is something wrong with him. Physically wrong, I mean. I don’t know what it is, but I am satisfied that it goes far beyond his ball-playing. I have seen ballplayers ‘go’ overnight, as Gehrig seems to have done. But they were simply washed up as ballplayers. It’s something deeper than that in this case, though.”
A hot topic in the field of motor neurodegeneration relates to the potential role of exercise.
On the one hand, patients are desperate for information, particularly in regards to potential lifestyle-related benefits of exercise. Conversely, clinicians and scientists continue to argue over a potential role for exercise in terms of disease causation.
Unfortunately, these are complex, largely unresolved areas of debate, and so the potential benefits of exercise in ALS remain an open discussion between physician and patient.
In America, motor neurone disease (or amyotrophic lateral sclerosis) is also known as Lou Gehrig’s disease, named after the famous New York Yankees baseballer (figure). Gehrig was a superb athlete, and as with most MND/ALS patients, there seemed to be no apparent reason for him to contract this universally fatal disease at the young age of 35, to die two years later.
Other seemingly random cases have subsequently been described in high performance athletes. A retrospective study of more that seven thousand footballers from the Italian professional leagues established that standardized morbidity ratios were increased for the development of MND/ALS, particularly younger onset (Chiò et al, 2005). For unexplained reasons, footballers who played for more than five years, particularly in an active midfield position, were at highest risk.
Other studies have suggested a raised risk of ALS in marathon runners, and further epidemiological investigations are currently underway in rugby populations.
Although MND/ALS is typically sporadic, approximately 5-10% of cases are familial, whereby two or more family members are clinically affected. The exact pathophysiological mechanisms underlying neurodegeneration in familial and sporadic MND/ALS have yet to be defined. Inheritance of familial MND/ALS is usually autosomal dominant, often linked to mutation of the copper/zinc superoxide-dismutase-1 gene (SOD-1) resulting in the typical adult-onset MND/ALS phenotype. The key function of the SOD-1 enzyme involves free radical scavenging, with the enzyme catalyzing the conversion of the superoxide anion to molecular oxygen and hydrogen peroxide.
The processes underlying MND/ALS appear multifactorial, involving complex interaction between genetic factors and molecular pathways, with resultant damage of critical target proteins within the motor neurone. In terms of any pathophysiological link between exercise and the development of MND/ALS, oxidative stress, excessive free radical production, and increased glutamate stimulation may all accompany normal motor neurone activation. However, it is plausible that such processes may potentially become neurotoxic as a result of exercise and excessive activition in susceptible individuals.
Dysfunction of the energy-dependent, axonal Na+/ K+ electrogenic pump may also be an integral factor contributing to motor neurone loss in MND/ALS. In addition to regulating the resting membrane potential, the axonal membrane electrogenic pump exerts a significant role in the restoration of gradients after high-frequency impulse activity, as presumably occurs with exercise. Overactivity of axonal Na+/ K+ pump, in the setting of progressive weakness in ALS, is likely to be a significant contributing factor to the common symptom of fatigue (Vucic et al., 2007).
However, this discussion remains largely hypothetical and relates more to a potential role for exercise in the causation of MND/ALS.
What advice then should a neurologist provide to patients once diagnosed with MND/ALS regarding their lifestyle and specifically, the role of exercise? Unfortunately a Cochrane analysis cited a lack of randomised clinical trial data that may guide appropriate discussion concerning the potential benefits or risks of aerobic type exercise in MND/ALS (Dalbello-Haas et al, 2008).
Similarly, there is limited information concerning resistance training, although recent pilot studies involving inspiratory muscle training suggest potential benefit, with larger multicentre studies currently underway (Cheah et al, 2009).
To further muddy the waters, findings in animal models of ALS have been inconsistent. Criticially, these type of studies must be interpreted with caution, particularly in relation to human disease, given the fact that of the many (> 100) trials undertaken in SOD-1 mouse models of MND/ALS, none of the positive findings from animal studies have translated into meaningful therapy in human MND/ALS.
Any suggestions of a potential role for exercise in either disease causation, or alternatively and somewhat conversely, therapeutic intervention, clearly need further validation.
Discussion may serve to increase the momentum for larger scale, exercise-based clinical trials in MND/ALS patients.
If you have an opinion, let us know!
References:
Cheah BC, Boland RA, Brodaty NE, Zoing MC, Jeffery SE, McKenzie DK & Kiernan MC. (2009). INSPIRATIonAL – Inspiratory muscle training in amyotrophic lateral sclerosis. Amyotroph Lateral Scler 10(5-6):384-392.
Chiò A, Benzi G, Dossena M, Mutani R & Mora G. (2005). Severely increased risk of amyotrophic lateral sclerosis among Italian professional football players. Brain 128, 472-6.
Dalbello-Haas V, Florence JM & Krivickas LS. (2008). Therapeutic exercise for people with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database Syst Rev 16, CD005229.
Vucic S, Krishnan AV, Kiernan MC (2007). Fatigue and activity-dependent changes in axonal excitability in ALS. J Neurol Neurosurg Psychiatry 78, 1202-1208.