Professor El-Omar has chosen Dr Daniel So, Professor Peter R Gibson and Associate Professor Jane G Muir, from the Department of Gastroenterology, Monash University and Alfred Health Hospital, Melbourne, Victoria, Australia, to do the next #GUTBlog.
The #GUTBlog focusses on the latest paper “Dietary fibres and IBS: translating functional characteristics to clinical value in the era of personalised medicine” which was published in paper copy in GUT in December 2021.
The team write:
The ‘traditional’ idea (one that is still prevalent) was that fibres, in general, would act as bulking agents to reduce symptoms by ameliorating disorders in motility, which at that time, was thought to be the main pathophysiological factor of IBS (1). In that way, fibre supplements would improve symptoms in general. The reality, however, was that fibre supplementation had very modest or no effects on symptoms in clinical trials and that changes in motility did not occur in parallel with changes in symptoms. Interest waned 30 years ago, partly related to the disappointing results and partly to distraction from fibre by prebiotics and FODMAPs (see below). The output of clinical research studies runs in waves as shown in figure 1. Fibre is undergoing its second wave after a hiatus of 15 years.
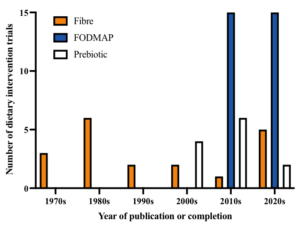
Figure 1.Trends in dietary intervention trials in irritable bowel syndrome, adapted from Dimidi et al. (2). Data for prebiotic trials obtained from Wilson et al. (3) and for more recent trials, registrations from clinical trial registries.
This reawakening was driven by several advances in the field. First, it became apparent that the concepts of ‘soluble’ fibre and ‘insoluble’ fibre were outdated and did not convey the functional effects of individual fibres. Instead, fibres should now be described by their ability to bulk the stool, their gel-forming effects and their susceptibility to fermentation (breakdown) by bacteria. Secondly, our understanding of what was actually going on in the body in IBS underwent a revolution with disordered motility taking a backseat to concepts that included disordered gut-brain axis, heightened gut sensitivity (known as visceral hypersensitivity), mild inflammation in the gut and greater understanding of the key roles that the gut microbiota has in IBS and gut health. Thirdly, developments in microbiome science, which have revealed the multiple ways that specific fibres can impact the gut microbiota via fermentation, and how the metabolites produced, such as gases and short-chain fatty acids, impact physiology. Fourthly, the concept of dietary FODMAPs (poorly absorbed small-molecule carbohydrates, like fructose and fructans) was introduced and the success of reducing their intake on IBS symptoms refocussed attention to carbohydrates and the different ways they interact with microbiota and the contents of the bowel. Finally, the emergence of technologies capable of providing information on what fibres were doing in different parts of the gut. For example, magnetic resonance imaging techniques have highlighted how two very different fibres such as inulin and psyllium influence the water and gas content of the small and large bowel, and how the two fibres interact when used in combination (4). Likewise, novel telemetric capsule techniques – the wireless motility capsule and the experimental gas-sensing capsule, where a capsule is swallowed and sends information from around the gut to an external receiver – provide a glimpse from inside to determine how fast contents are moving, and to define pH or gas concentrations within specific regions of the gut. Such techniques are setting the scene to enable personalisation of the type of fibre to be used. In other words, treatment decisions in a person with IBS may be directed by the individual’s physiology.
While we have speculated that the future of fibre supplementation will be individualised according to the physiology and other characteristics of the patient rather than just their symptom pattern (as is now done), many further studies are needed to translate such ideas into actual clinical practice.”
References
- Drossman DA, Thompson WG. The irritable bowel syndrome: review and a graduated multicomponent treatment approach. Ann Intern Med1992;116:1009-16. https://doi.org/10.7326/0003-4819-116-12-1009
- Dimidi E, Rossi M, Whelan K. Irritable bowel syndrome and diet: where are we in 2018? Curr Opin Clin Nutr Metab Care 2017;20:456-63.https://doi.org/10.1097/MCO.0000000000000416
- Wilson W, Rossi M, Dimidi E. Prebiotics in irritable bowel syndrome and other functional bowel disorders in adults: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr2019;1098-111. https://doi.org/10.1093/ajcn/nqy376
- Gunn D, Abbas Z, Harris HC et al. Psyllium reduces inulin-induced colonic gas production in IBS: MRI and in vitro fermentation studies. Gut 2021;0-9. https://doi.org/10.1136/gutjnl-2021-324784