by Sinead Cook
People who attend Sexual Assault Referral Centres (SARCs) have a variety of acute and longer-term sexual health and contraceptive needs. In Cardiff, we introduced a local policy in 2017 that aimed to ensure high-quality immediate care within the SARC and onwards referral to the local integrated sexual health clinic. A year later, we conducted an audit to ascertain if the introduction of this protocol had been successful in meeting patients’ acute sexual health and contraception needs after sexual assault. We reviewed 32 SARC and sexual health case notes of adults who attended the SARC between 1 April – 1 July 2018.
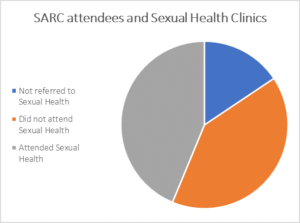
We were surprised to discover that while most SARC patients (27/32) are referred to sexual health clinics, many (13/27) don’t attend.
This is despite our sexual health clinic being co-located in the same building as the SARC and offering a ‘fast-track’ appointment for any patient referred from SARC. Furthermore, in the majority (10/13) of cases, the same patients did not engage with follow-up offered by the SARC. Importantly, among those attending, the rate of STIs appears high (2/14, 14%).
Our findings echo experience from other centres; the Haven reported that 45% of patients did not attend for any follow-up despite all follow-up being offered within the same setting, and in those that did and had an STI test, 12% were diagnosed with one or more infections.
Although Forensic Medical Examiners focus predominantly on identifying forensic evidence for the police, they acknowledged the importance of clients’ health needs. However, immediate care (in terms of emergency contraception, hepatitis B vaccination and HIV post exposure prophylaxis provision) within the SARC appeared variable and not consistently in line with national guidelines.
Our study has shown that the initial attendance at the SARC may be the only contact the patient has with health services and so needs to be optimised. We feel it is also important to improve follow-up attendance for STI testing as this population appears to have high levels of STIs. We are therefore implementing various changes to attempt to both improve care provided within the SARC and also sexual health clinic attendance.
Read the full article here: Cook S, Cunningham L, Mott A. Sexual healthcare and contraception provision after sexual assault. BMJ Sexual & Reproductive Health. 05 November 2019.