The direction of travel for the NHS is now clear. The three key themes are Hospital to Community, Treatment to Prevention and Analogue to Digital. But there is also an attendant theme, ubiquitous and permanent. How do we increase productivity and get the best outcomes from the £180Bn currently spent per annum on health and social care (2022/3) of which £155Bn was spent on the NHS in England?
Who is accountable for ensuring that these things happen? Who is accountable for bringing down waiting lists from 7.5M? Just stating a problem or aspiration gets us nowhere. All too often, reviews and reports designed to improve the structure and function of the NHS get no more than partially implemented before they are overtaken by the next iteration of the same review and report process. Democratic accountability through the ballot box is the bluntest of blunt instruments and useless for ensuring that NHS improvements are implemented. Replacing an entire government does not hold specific individuals or groups accountable for their actions. The law is a similar blunt instrument which is so drawn out that it can take many years for legal accountability to be enforced. Royal Commissions tend to be even worse.
Whilst it is clear that accountability needs to be exercised managerially in the running of the service, close to where the decisions are taken and implemented, this is exactly where the bureaucratic nature of the system is a key hindrance. We are convinced that if the answer to a problem is to form a committee, then we are almost certainly asking the wrong question. Yet committees abound in the running of the NHS and its associated bodies such as the professional colleges.
Committees can seem attractive. They involve many people in decision making and, when well-run, ensure that all aspects of an issue are considered. Yet when it comes to actually getting things done, they can be intrinsically inefficient and risk obscuring accountability by diffusing responsibility across large groups of participants. This reduces the probability that any individual is held accountable for decisions taken. Committees can also report to committees in a nested obfuscation that removes any vestige of accountability, a collusion of assumptions that because an issue has been discussed, action will follow.
Worse, many committees tend to multiply work, overwhelming their members with detail. One NHS organisation with which we worked regularly had to read 400+ pages of papers for their meetings. Whilst this is not uncommon it is certainly unhelpful. Worse still, bureaucratic structures effectively create a system in which many people can say NO to a proposal but few can say YES having been vested with the power to ensure that something happens. We have worked with many boards and this is frequently their chief complaint: that they are stripped of authority and the power to make things happen by the weight of oversight required. All too often the same issues and aspirations can be discussed meeting after meeting, with little progress being made.
How is accountability to be made clearer? And would this be a good thing in the context of the NHS? In the 1980s, Sir Roy Griffiths (CEO of Sainsbury’s) wrote a brief report to Margaret Thatcher extolling the virtues of general management for the NHS since his investigations had led him to ask ‘who is in charge?’ since, to him, leadership and management were unclear in the health service. Forty years later, have we made any progress on this?
In our view, Griffiths’ question is still relevant. In most non-NHS organisations, managers at all levels are given clear objectives expressed in terms of the outcomes they need to achieve. They are regularly appraised to monitor progress and then reviewed and held accountable at the end of the period for which the goals were specified. There is a great deal of difference between senior managers as to how monitoring is done and the degree of freedom afforded to those being managed, but the principle is clear. All this stands as distinct from the role of most committees which tends to focus disproportionately on process. They focus not on performance but conformance.
There are various mechanisms for treating aims differently according to their nature. One we have used (Pendleton et al 2021) is a power-shift model, thus:
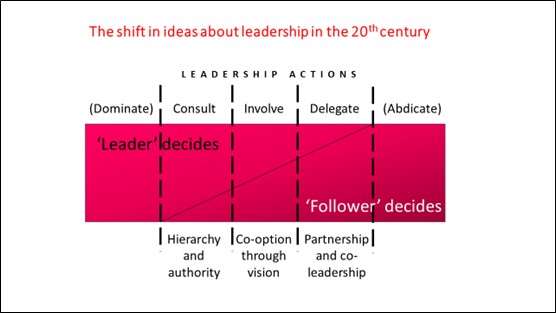
As leadership practices evolved in the 20th century, the norm shifted from left to right. The formal authority of the 19th century gave way gradually through the 20th century to more of a partnership model even raising the possibility of self-governing teams in which the leader can delegate or even abdicate from time to time. In current times, we are left with different types of leadership or managerial actions, especially Consult, Involve and Delegate. When a leader/manager consults on an issue, he or she will seek the views of others but reserves the right to make the final decision. If others are involved, then the decision is made together. If a matter is delegated, then the framework may be set (goal, timescale, required outcomes) and a means for monitoring and reviewing is agreed.
The key is to be clear about which matters will be handled in these specific ways. Once there is clarity, there is an explicit understanding about how accountability is to be managed. There is also a tendency increasingly to advocate delegation as frequently as possible to ensure a minimum of demotivating micro-management.
A similar method is dubbed RACI in which any allocated task has to specify who is Responsible, who is Accountable, who needs to be Consulted and who Involved. In this method, there may be multiple names in each category but the more there are, the more the potential for obfuscation.
Whilst some committees will have a valuable place in looking retrospectively at issues such as quality of care, when it comes to introducing new projects or new approaches we would love to see one or other of these methods, or something similar, replace most committees on most subjects. If consultation has to be extensive, then it needs to be done specifically and systematically. But decision making is not a strength of bureaucracies. Efficiency or productivity improvements are likely to need clear and distinct roles, the ability to make decisions and willingness to be accountable for them.
In the words of the Department of Health and Social Care (2020) Each part of the system must question and call out organisational habits or local rules which increase excess bureaucracy. Everyone needs to play their part in busting bureaucracy, from national government to local providers and frontline staff.’
Would it make sense to think through how England’s 42 Integrated Care Boards could be deployed to tackle the 7.5M waiting for diagnosis or treatment? One possible model could be the way Bill Bratton (Commissioner of the New York City Police Department) tackled crime in New York City: by making the precinct commanders accountable and providing the detailed and accurate information on which their performance could be judged. And if not, why not?
References
Bill Bratton and Peter Knobler (2021) The Profession. London and New York, Penguin.
David Pendleton, Adrian Furnham and Jon Cowell (2021) Leadership: no more heroes. London, Palgrave Macmillan
DHSC (2020) Busting Bureaucracy.
Authors
David Pendleton
David is a Professor in Leadership at Henley Business School and an Associate Fellow at Green Templeton College Oxford.
David Haslam
David is past Chair of NICE and Past President, RCGP.
Declaration of interests
We have read and understood the BMJ Group policy on declaration of interests and declare the following interests: none.